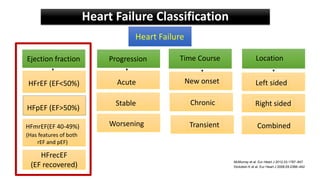
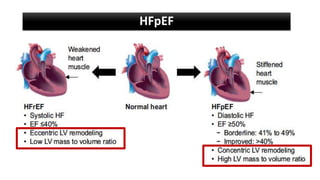
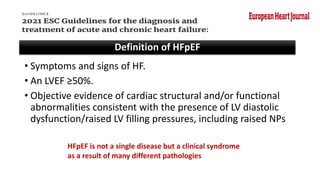
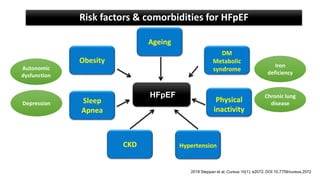
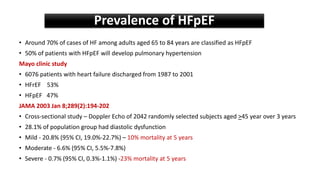
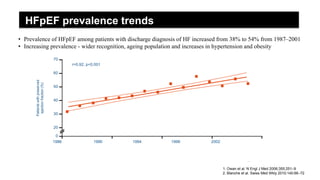
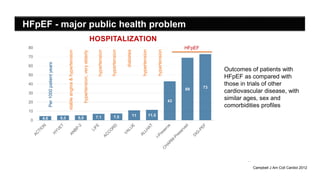
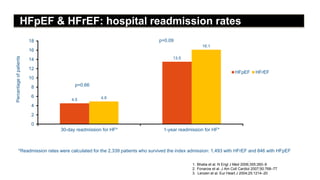
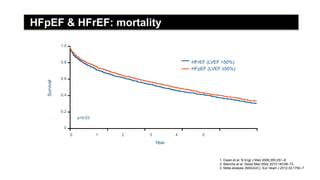
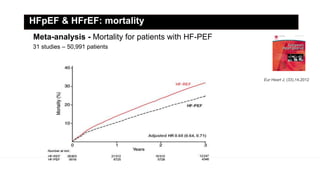
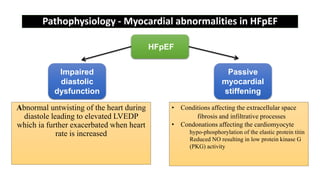
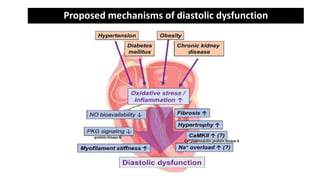
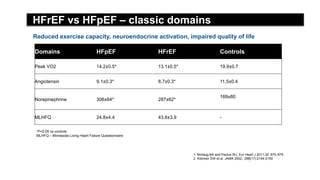
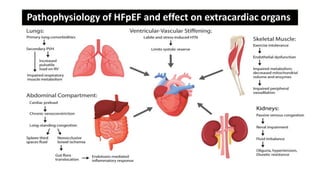
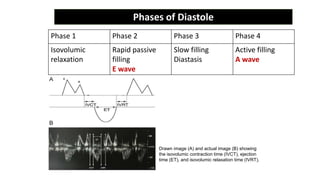
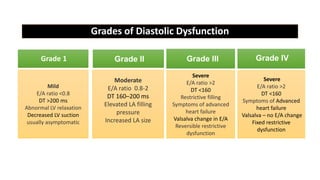
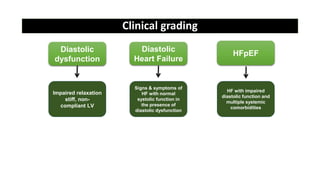
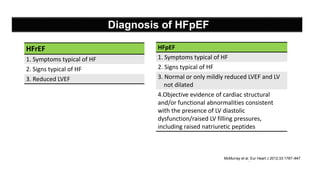
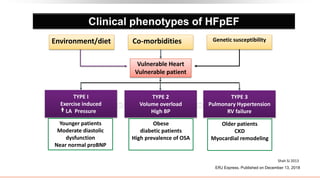
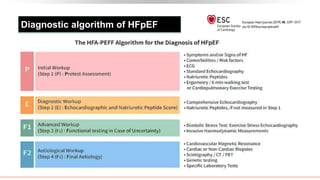
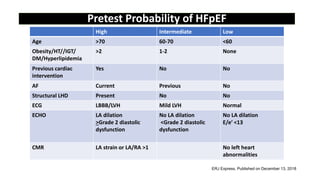
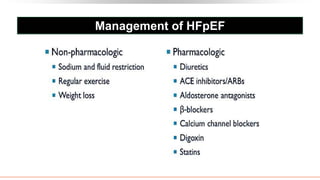
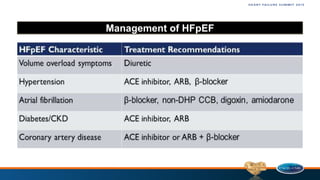
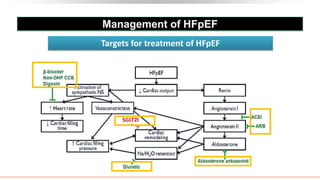
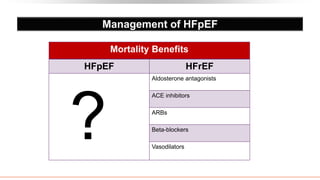
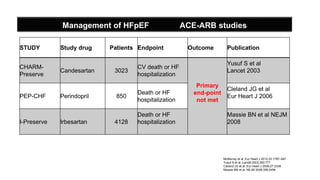
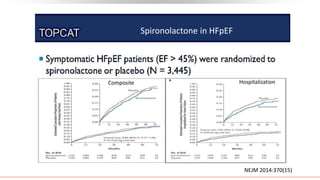
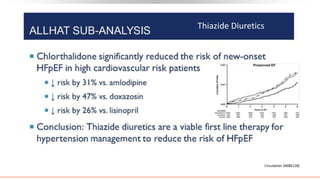
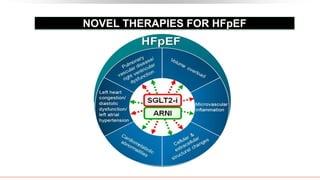
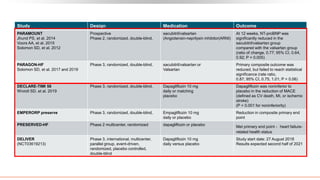
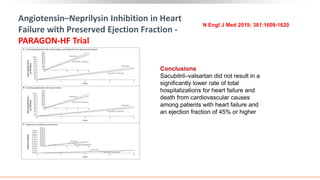
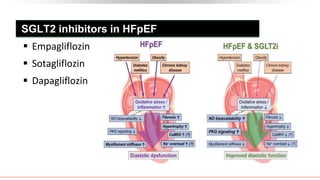
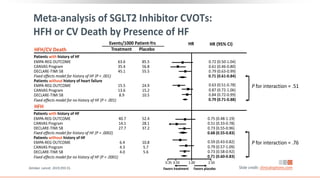
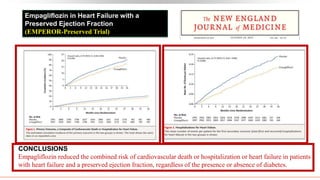
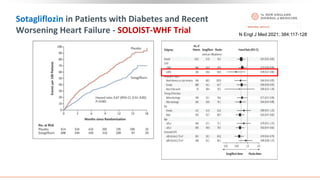
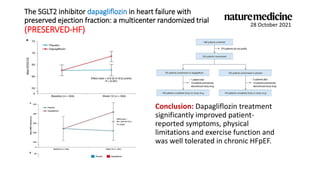
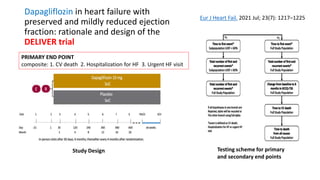
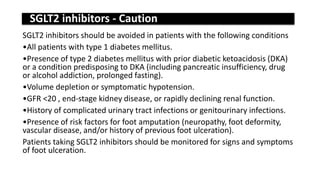
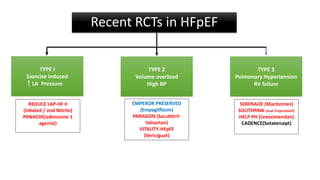
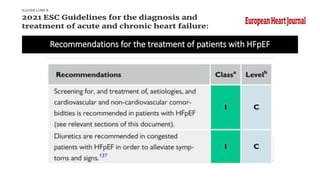
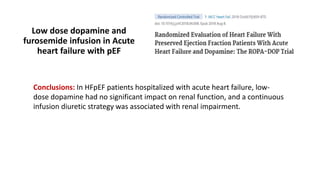
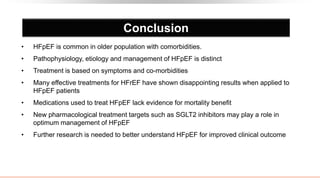
Heart failure with preserved ejection fraction (HFpEF) is a significant clinical syndrome characterized by symptoms of heart failure alongside an ejection fraction of 50% or greater, commonly associated with various comorbidities such as obesity and hypertension. The prevalence of HFpEF is increasing, particularly among older adults, affecting nearly 70% of cases in those aged 65 to 84, and it poses major challenges in terms of hospitalization and mortality rates akin to heart failure with reduced ejection fraction (HFrEF). Diagnosis involves evidence of diastolic dysfunction, and management focuses on optimizing fluid balance and treating associated conditions, with emerging therapies like SGLT2 inhibitors showing promise in improving outcomes.