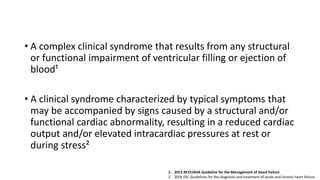
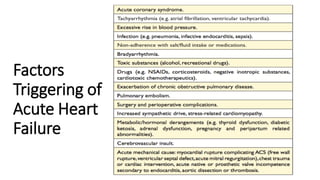
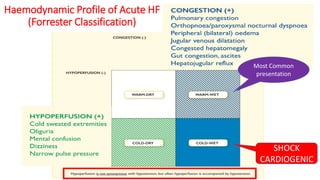
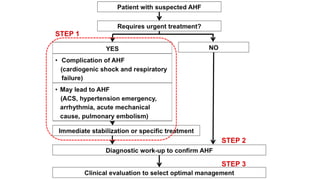
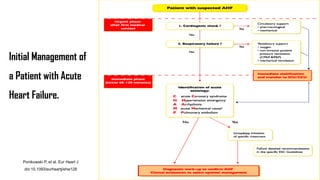
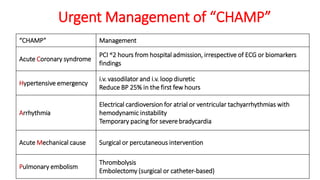
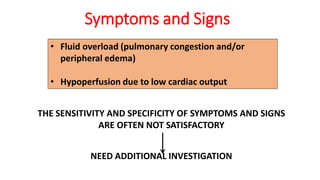
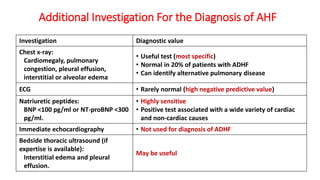
1. Acute heart failure is a life-threatening condition requiring urgent evaluation and treatment based on the patient's clinical profile and symptoms of fluid congestion or hypoperfusion.
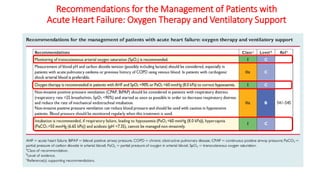
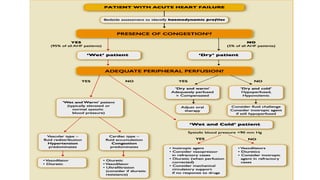
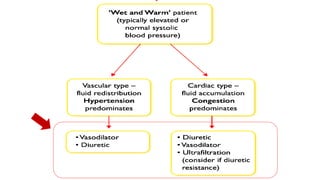
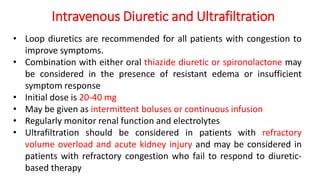
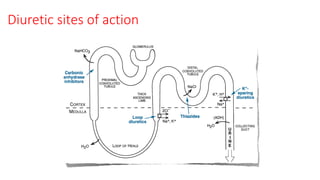
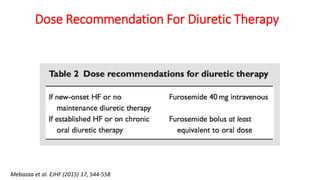
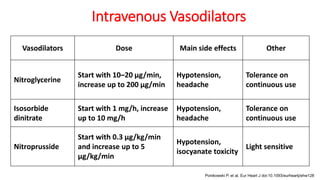
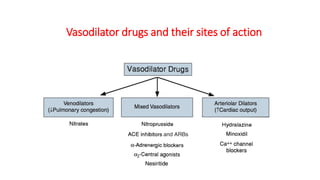
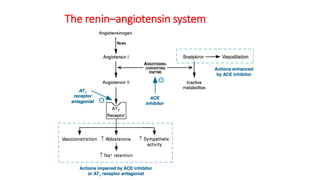
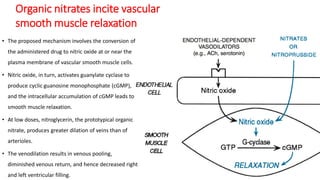
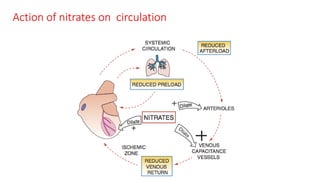
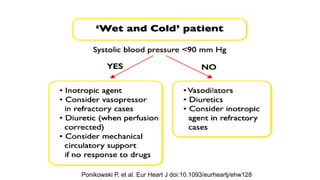
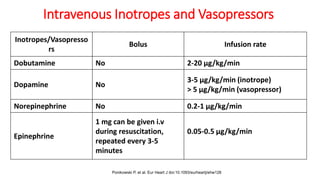
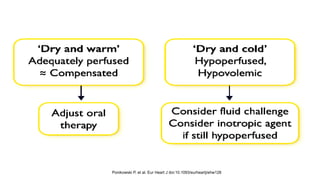
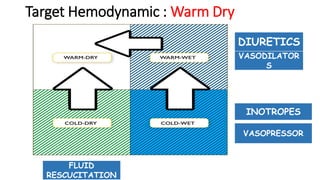
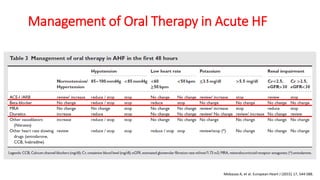
2. Initial management in the hospital involves intravenous diuretics and vasodilators to reduce fluid overload, along with inotropes or vasopressors if needed to support blood pressure and organ perfusion.
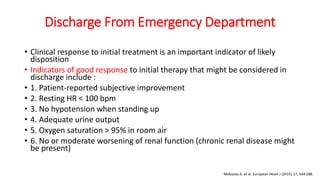
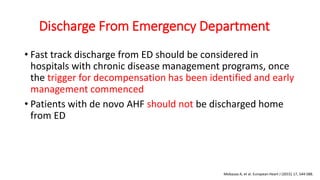
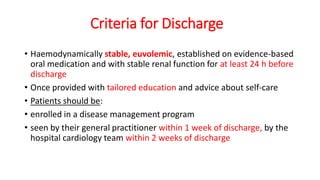
3. Patients are monitored closely and stabilized through optimization of therapy before being discharged with guidelines for follow-up and enrollment in disease management programs.