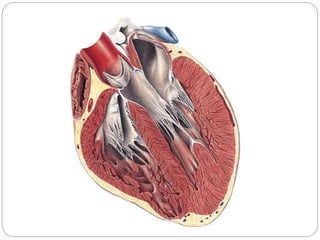
The document discusses the anatomy and physiology of the heart. It describes the heart's location and coverings including the pericardium. It details the heart chambers including the atria which receive blood and the ventricles which pump blood out. It explains the pathway of blood flow through the two circuits, pulmonary and systemic. It outlines the heart valves and electrical conduction system. Finally, it discusses the cardiac cycle and factors regulating cardiac output such as preload, contractility, and afterload.