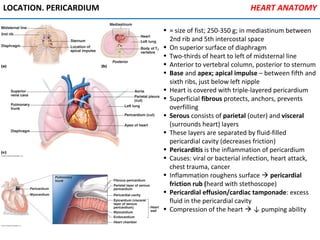
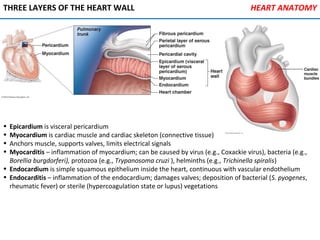
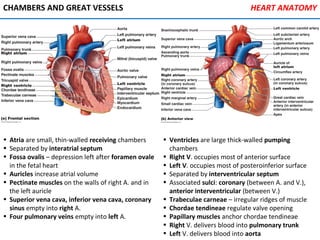
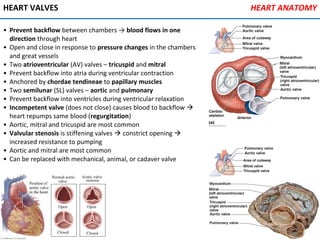
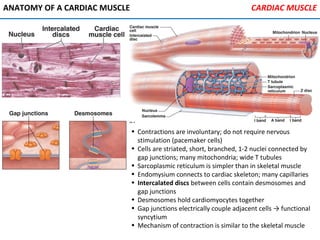
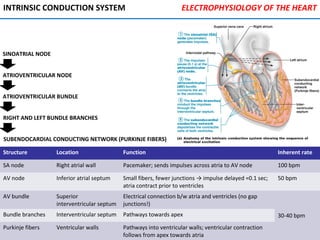
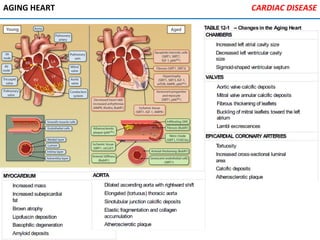
The heart is located in the mediastinum and is protected by the pericardium. It has four chambers - two atria that receive blood and two ventricles that pump blood out. The heart has three layers - the epicardium, myocardium, and endocardium. It is surrounded by the pericardium and has coronary arteries that supply its own blood flow. The heart has four valves that ensure one-way blood flow through the chambers and out to the lungs and body. It is able to contract rhythmically due to pacemaker cells that generate and conduct electrical signals.
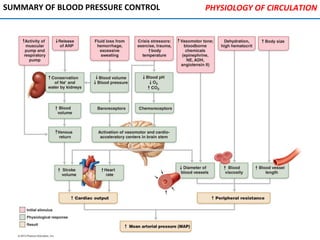
![PHYSIOLOGY OF CIRCULATION
Blood flow (BF) Volume of blood flowing through
vessel, organ, or entire circulation
in given period [ml/min]
Equivalent to cardiac output; constant at rest; local BF varies
between organs
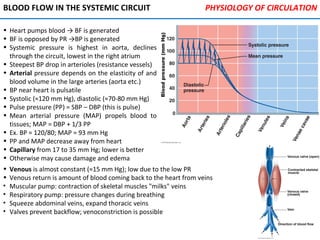
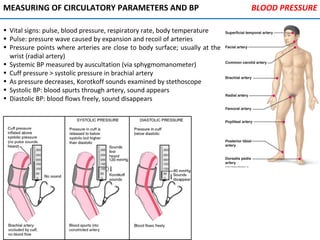
Blood pressure
(BP)
Force per unit area exerted on wall
of blood vessel by blood [mm Hg]
Measured as systemic BP in the large arteries; proportional to
blood volume (BV); blood follows pressure gradient (∆BP)
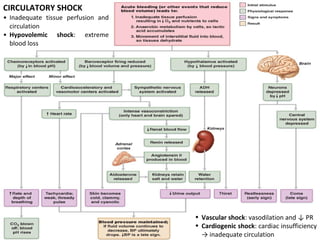
Peripheral
resistance (PR)
Opposition to flow Amount of friction blood encounters with vessel walls, generally
in peripheral (systemic) circulation
FLOW, PRESSURE, AND RESISTANCE](https://image.slidesharecdn.com/cardiovascularsystem-170116174108/85/Cardiovascular-system-46-320.jpg)