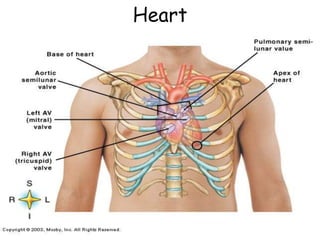
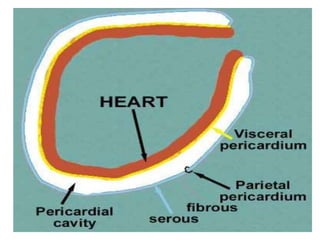
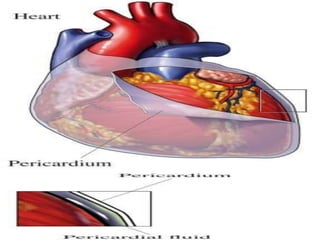
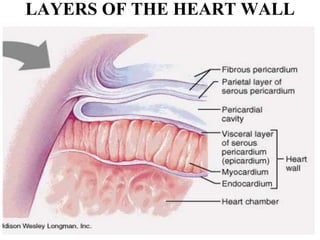
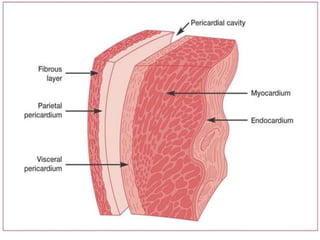
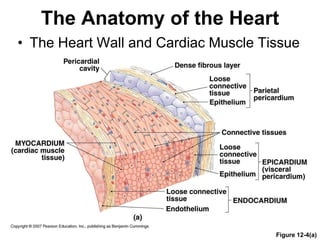
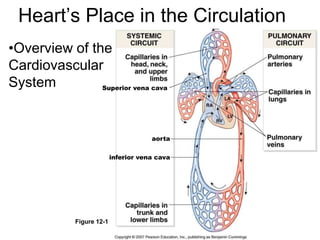
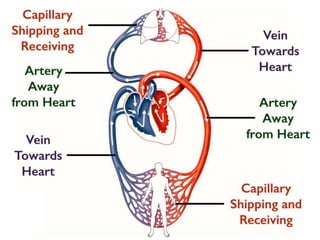
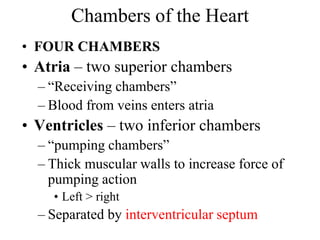
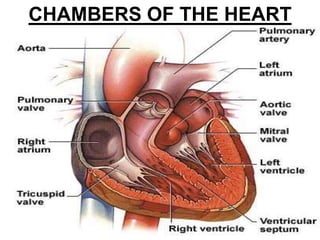
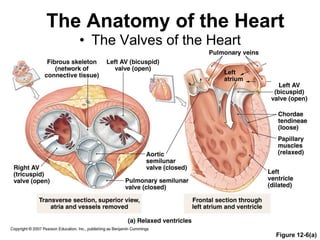
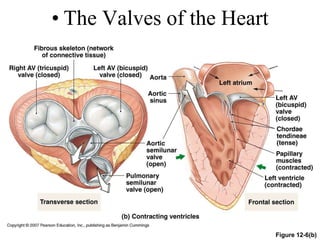
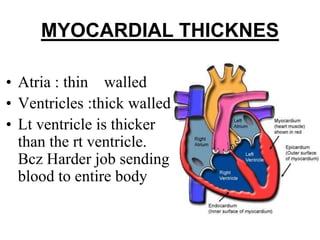
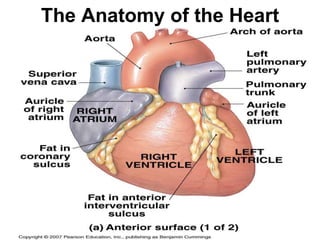
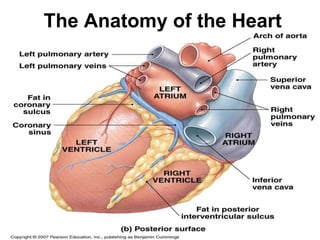
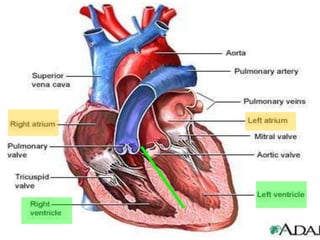
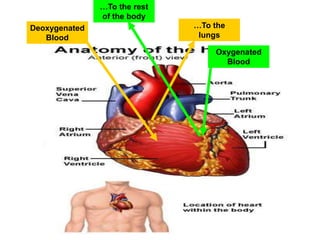
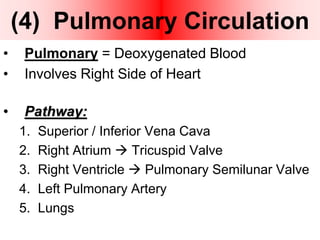
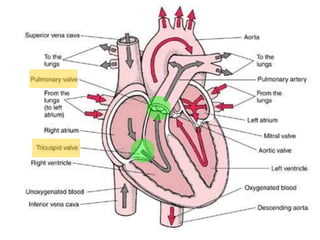
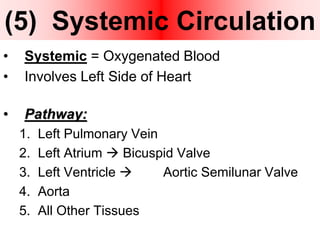
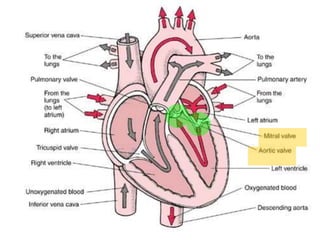
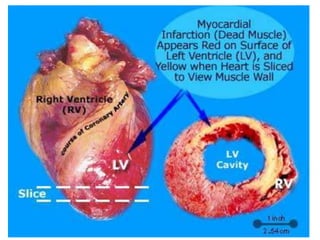
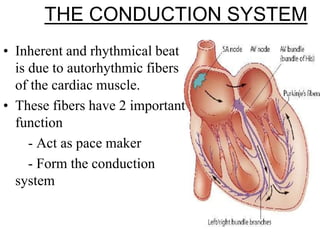
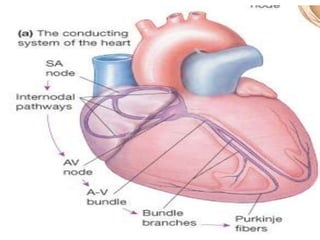
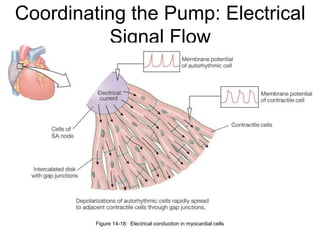
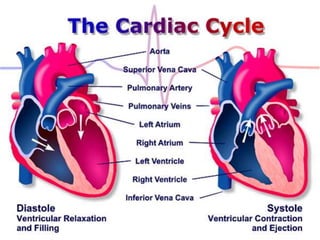
The heart is a four-chambered muscular organ located in the mediastinum protected by the pericardium. It pumps blood through two circuits - the pulmonary circuit to the lungs and systemic circuit to the rest of the body. The heart walls have three layers - epicardium, myocardium and endocardium. It has four chambers - two upper atria which receive blood and two lower ventricles which pump blood out. It uses valves to ensure one-way blood flow. The sinoatrial node initiates electrical impulses which coordinate contractions through the conduction system.