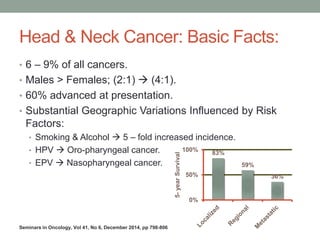
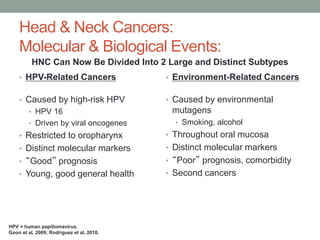
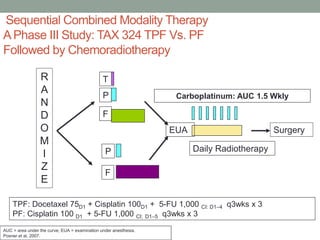
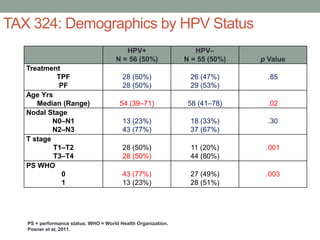
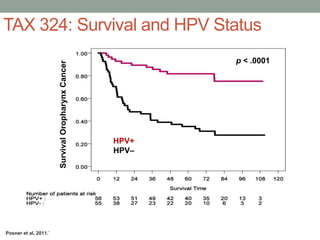
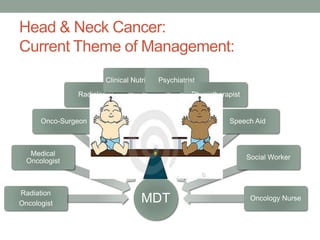
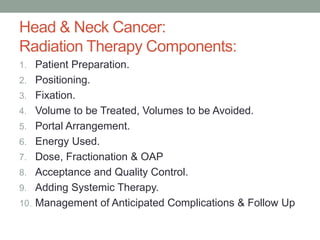
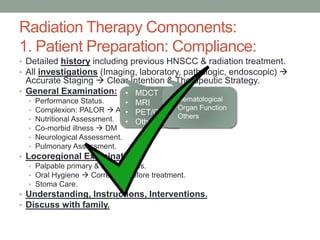
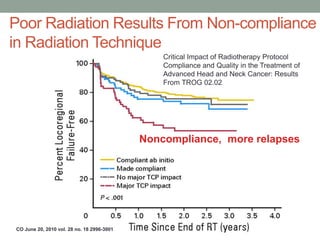
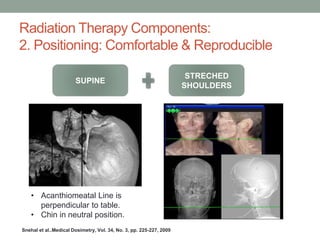
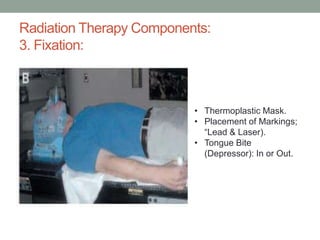
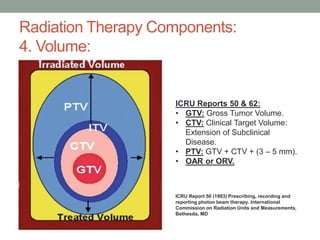
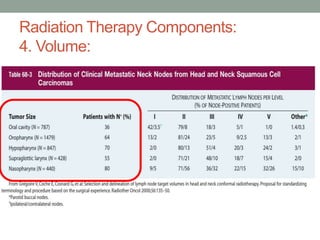
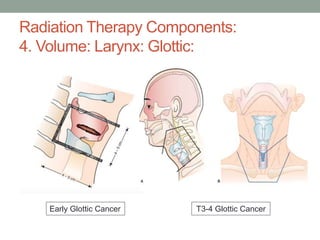
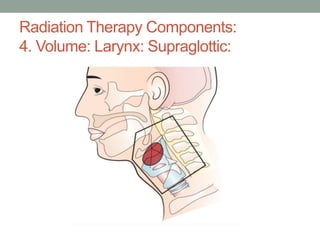
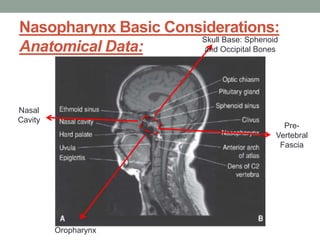
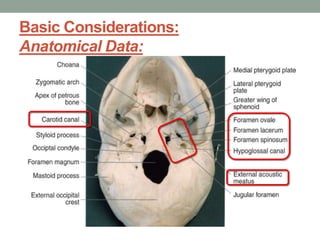
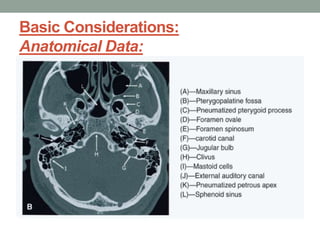
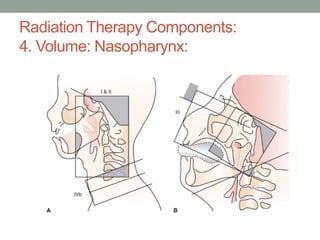
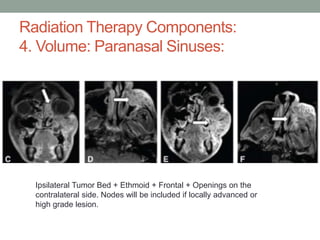
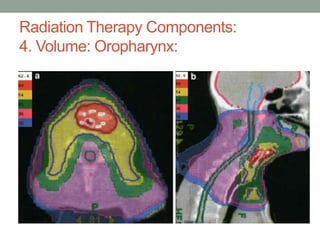
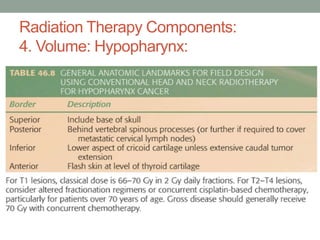
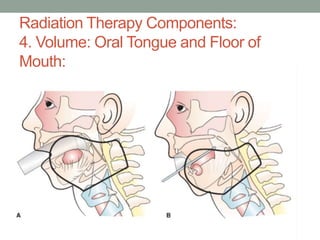
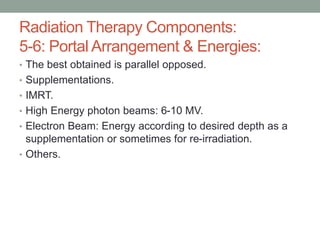
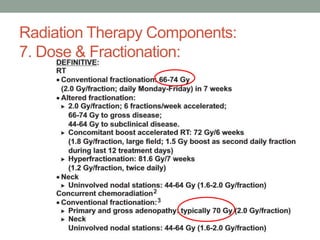
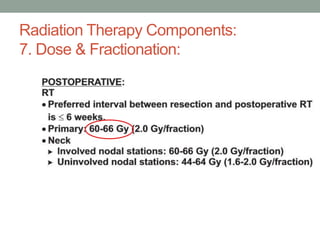
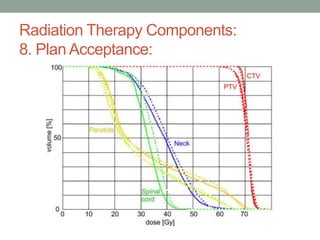
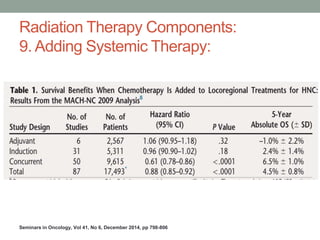
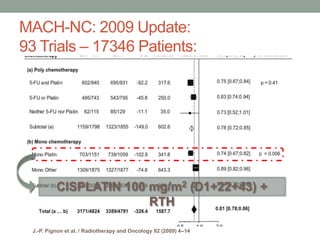
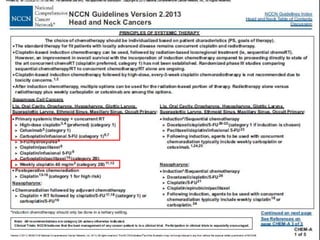
This document discusses head and neck cancer and radiation therapy. It provides background information on head and neck cancers, noting they make up 6-9% of cancers and are more common in males. Risk factors include smoking, alcohol, HPV, and EBV. It then discusses the components of radiation therapy planning and delivery in detail, including patient preparation, positioning, volume definition, portal arrangement, dose and fractionation, plan acceptance, adding chemotherapy, and managing complications. The importance of a multidisciplinary team approach is also emphasized.