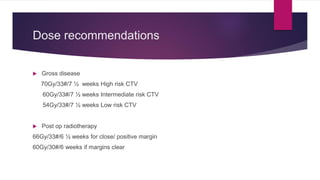
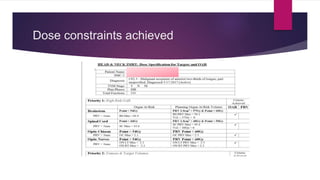
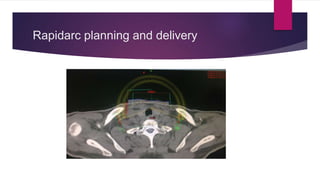
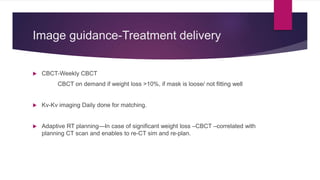
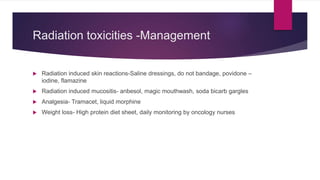
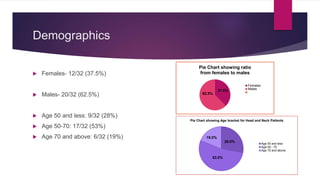
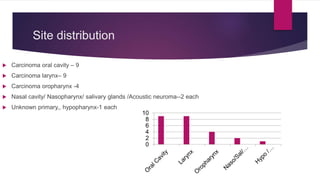
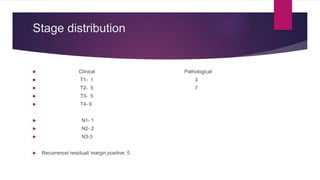
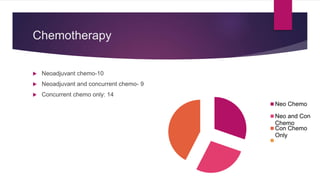
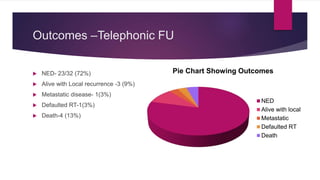
The document outlines techniques and challenges in the radiotherapy treatment of head and neck cancers, including the role of radiotherapy, chemotherapy, and various treatment modalities. It details the Southern Medical Clinic's experience with patient demographics, treatment outcomes, and the importance of timely diagnosis and management of side effects. Additionally, it highlights the workflow and protocols followed for effective radiation planning and delivery.