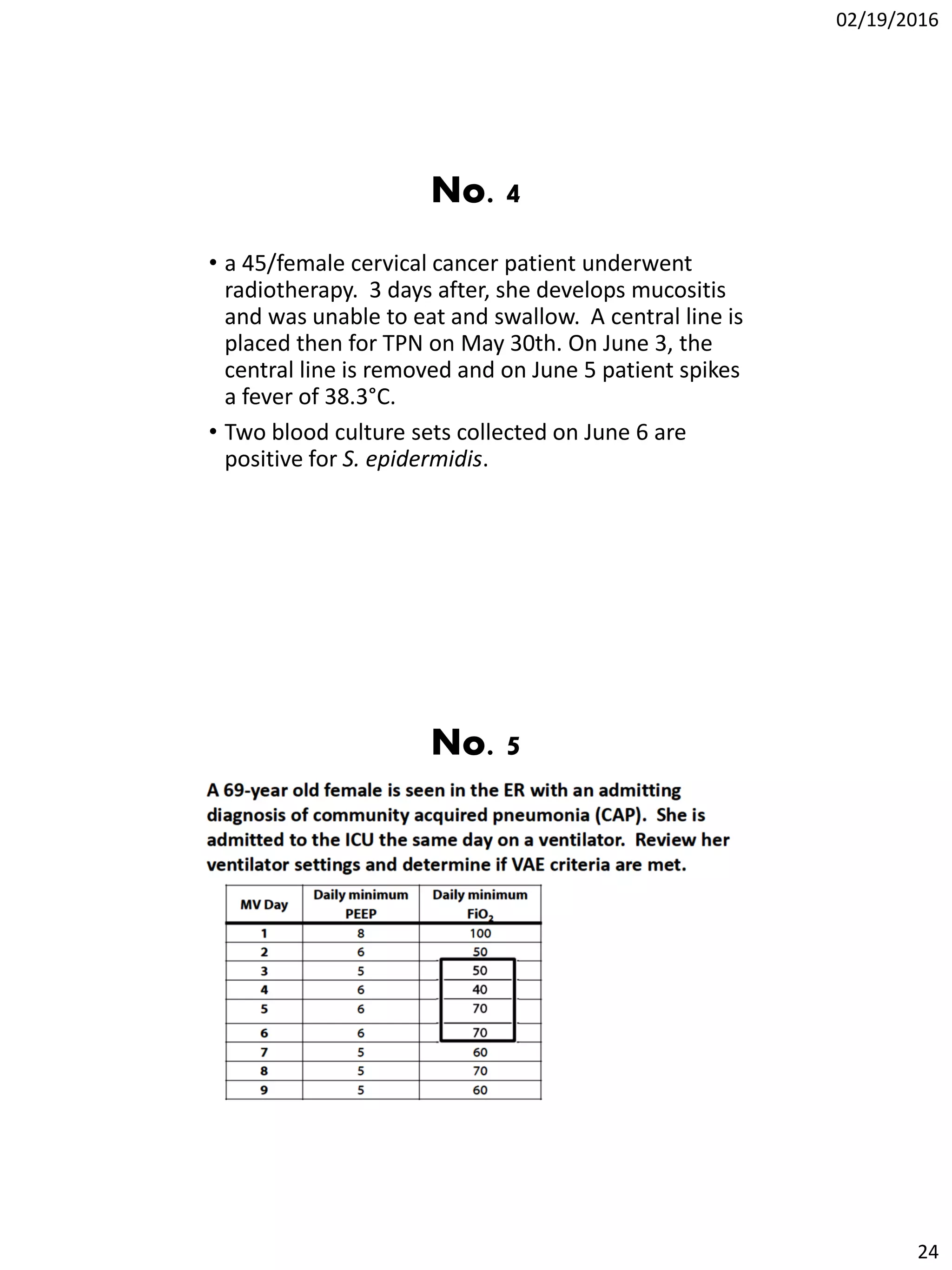
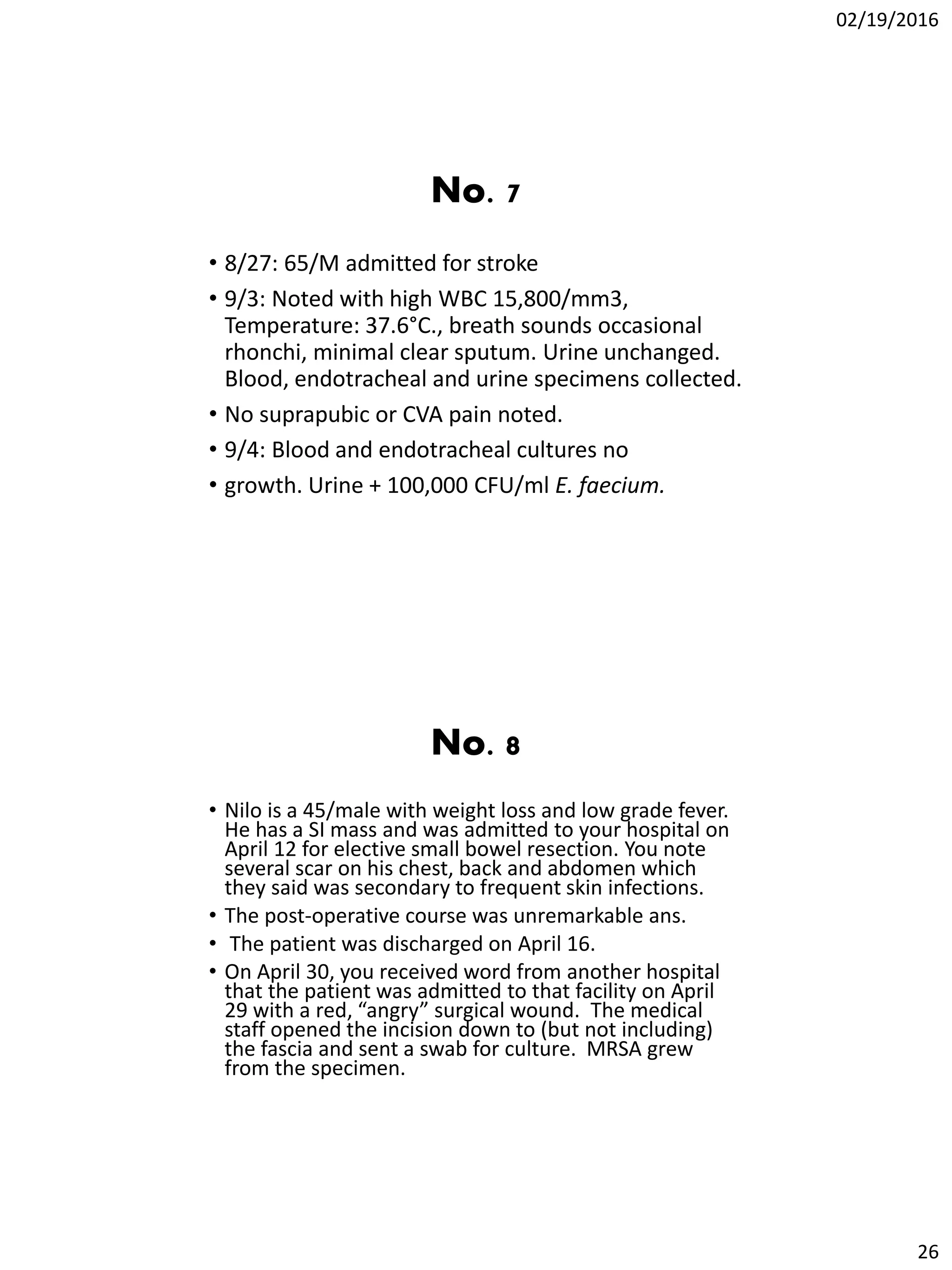
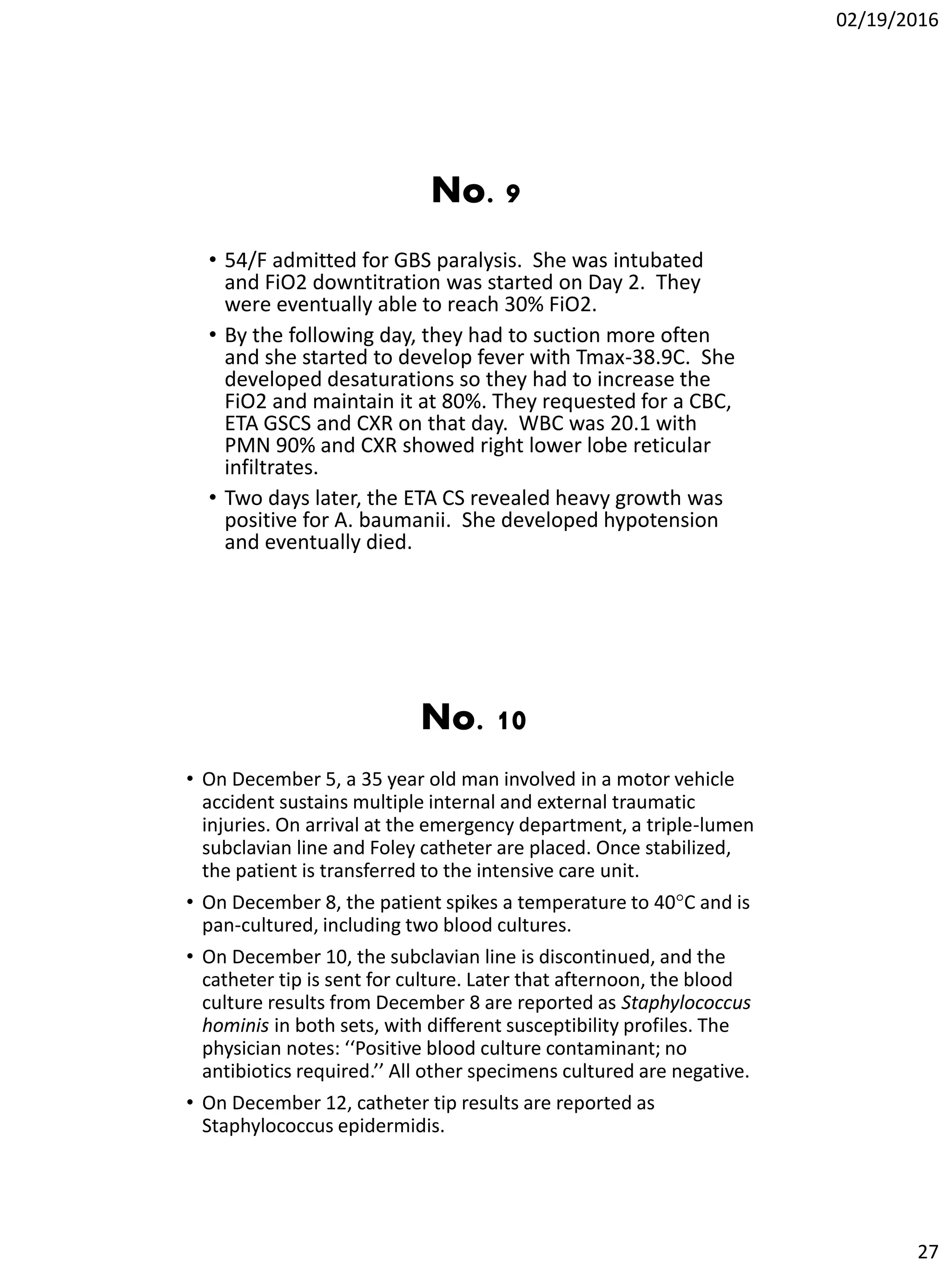
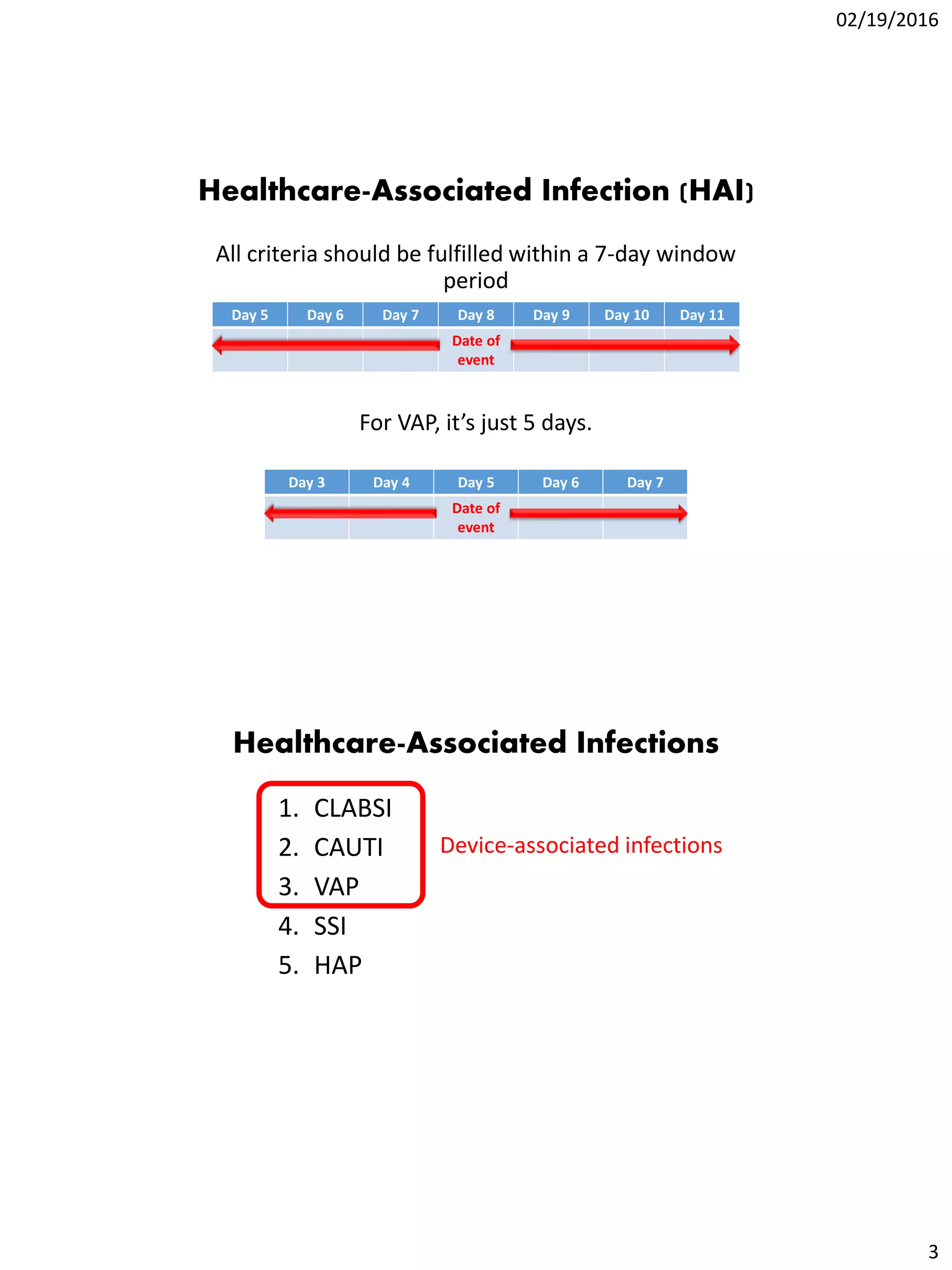
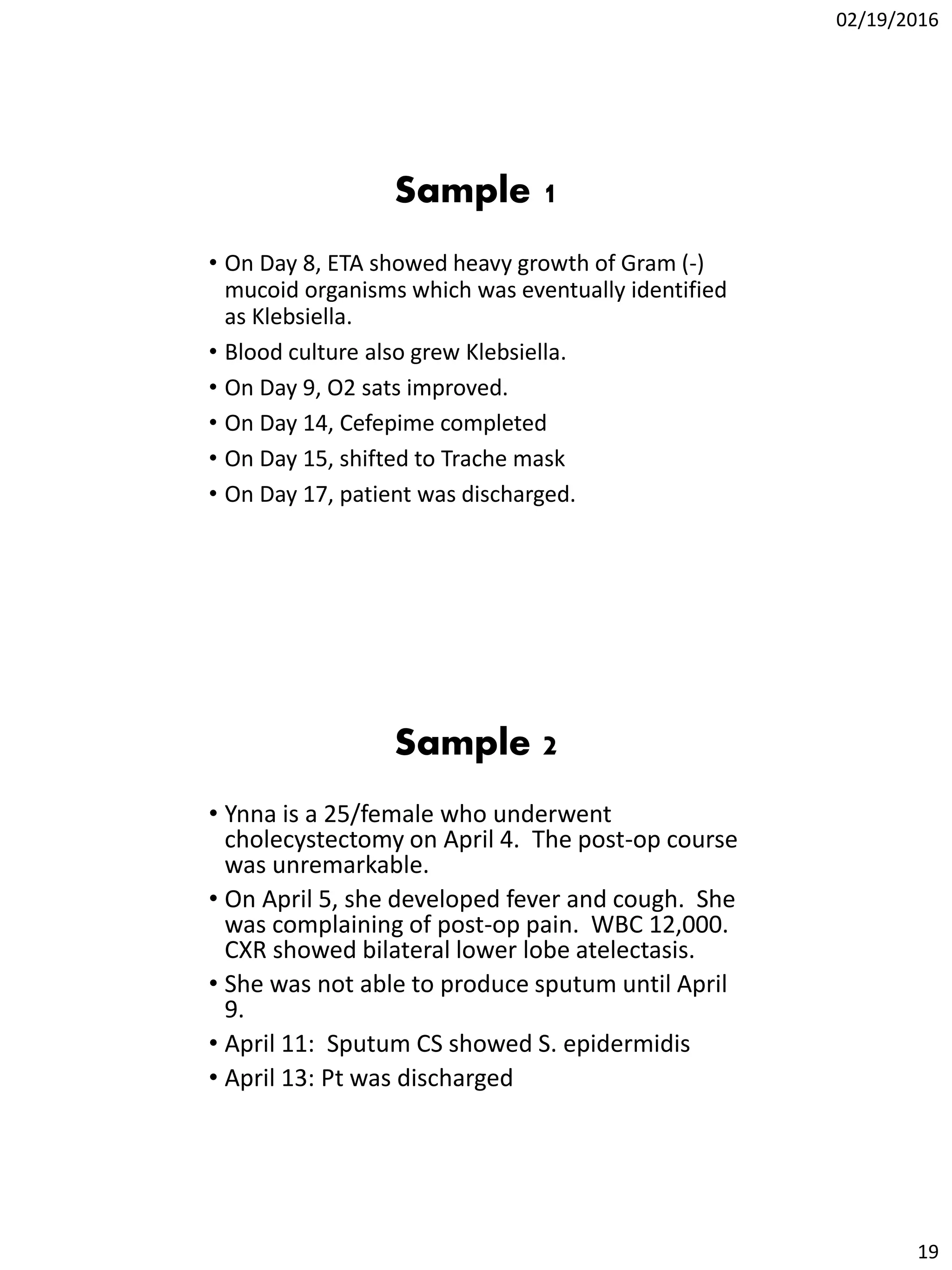
The document discusses definitions and standardizations for healthcare-associated infections according to the CDC and DOH, including defining infections like CLABSI, CAUTI, SSI, VAP, and HAP. It provides details on surveillance methods and criteria for determining if an infection meets the definition of these specific infection types. Examples are also given to demonstrate how to identify if a patient scenario represents one of these healthcare-associated infections.
![02/19/2016
6
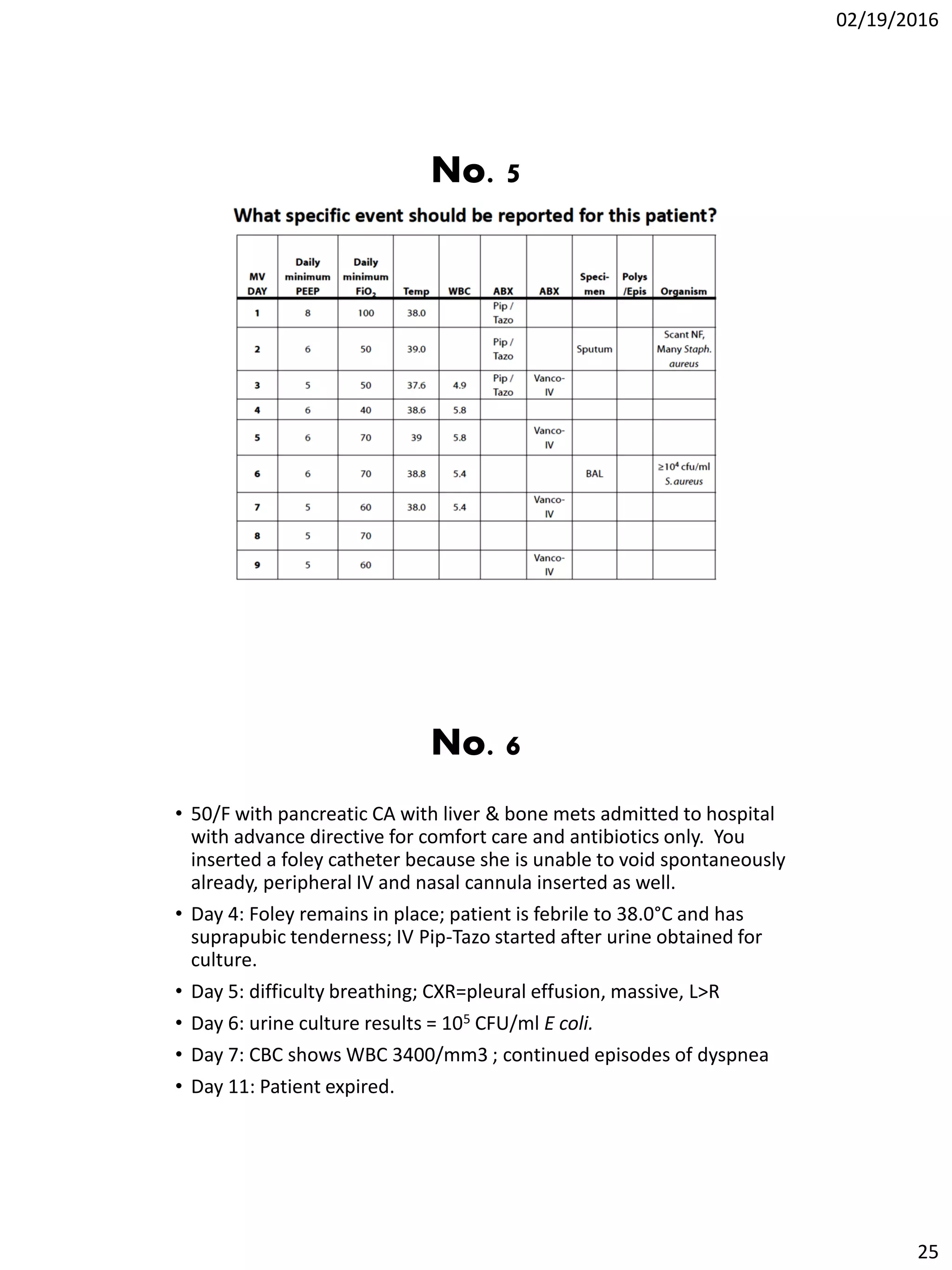
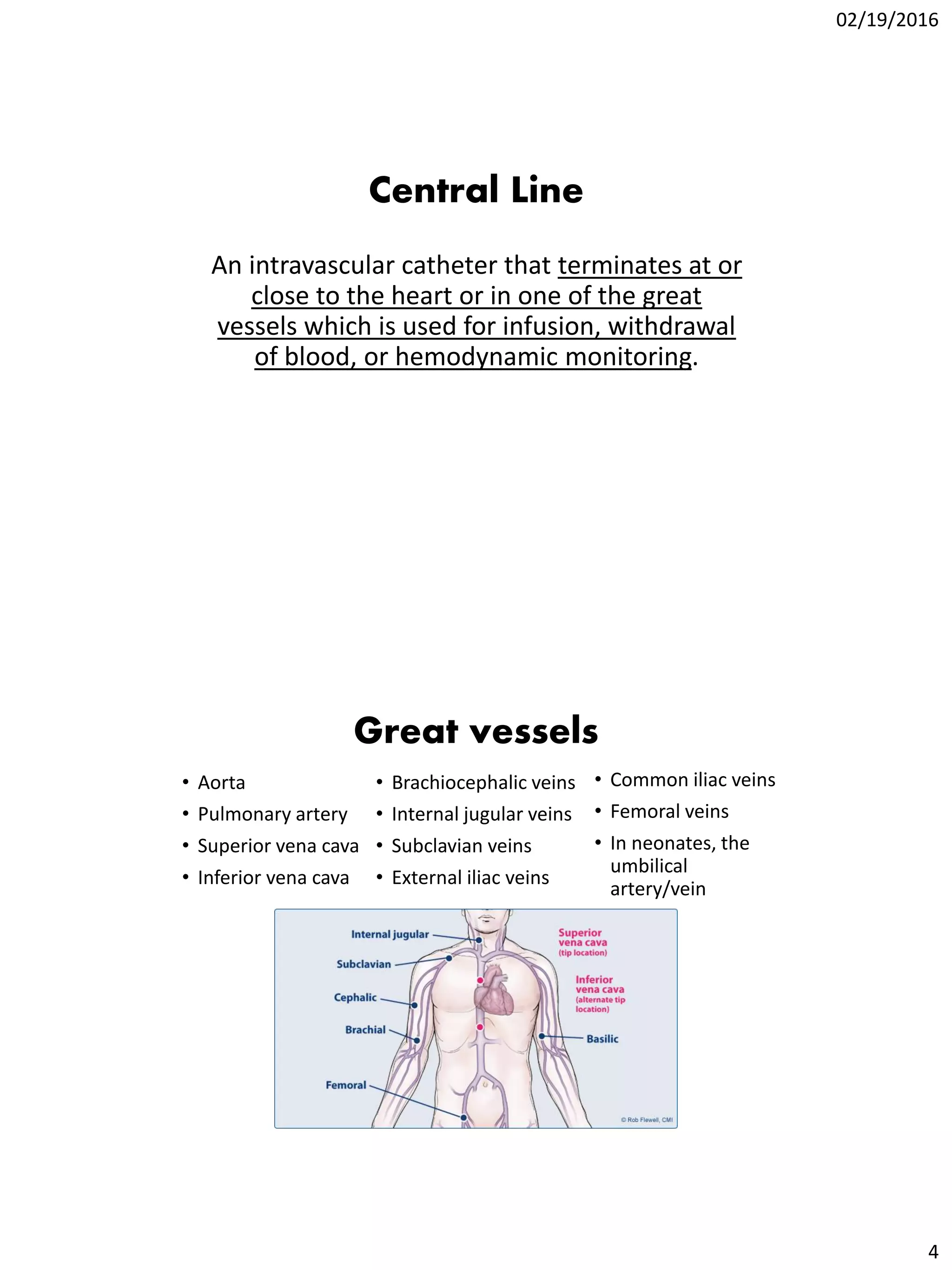
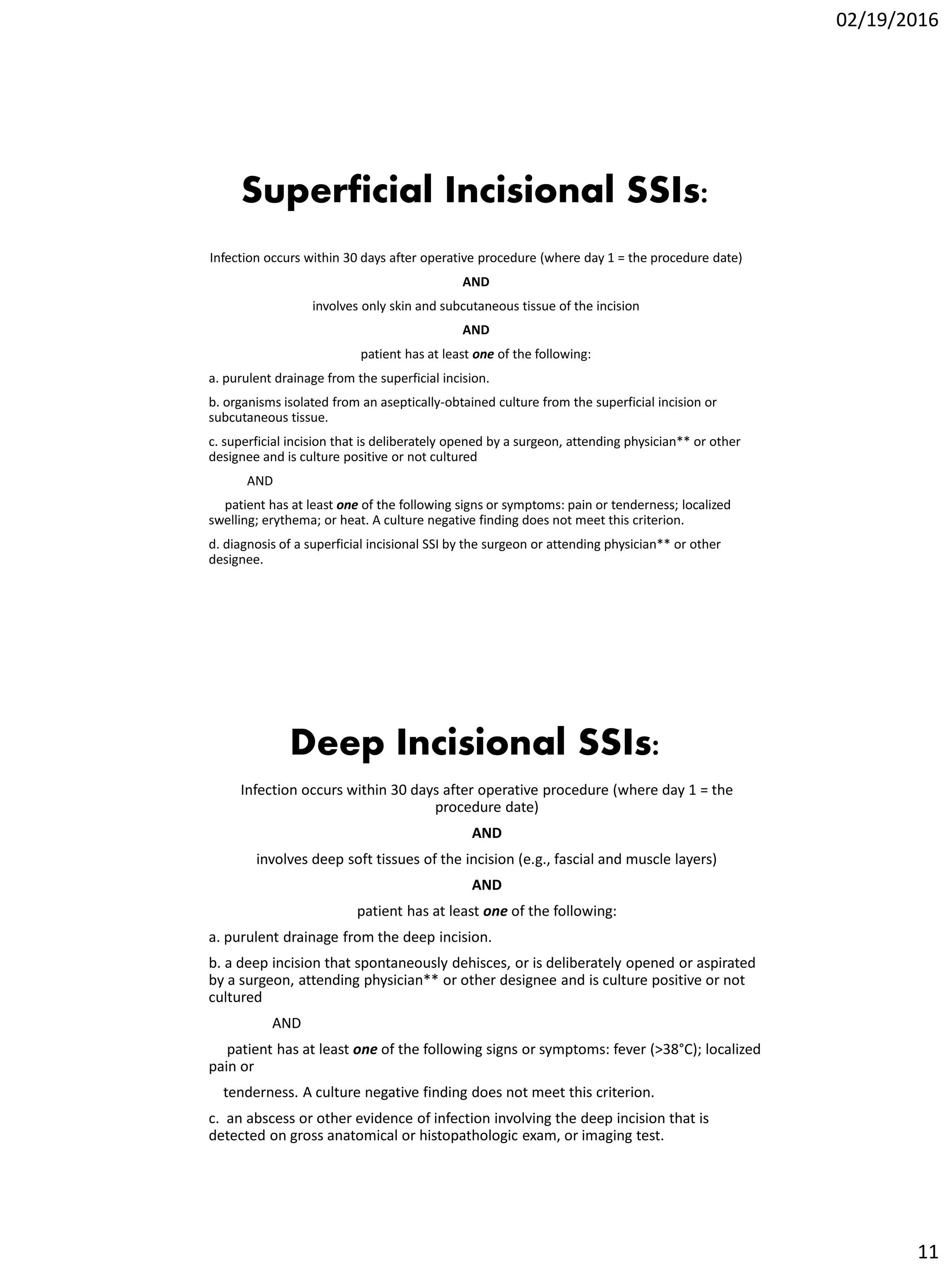
Central line-associated
bloodstream infection (CLABSI)
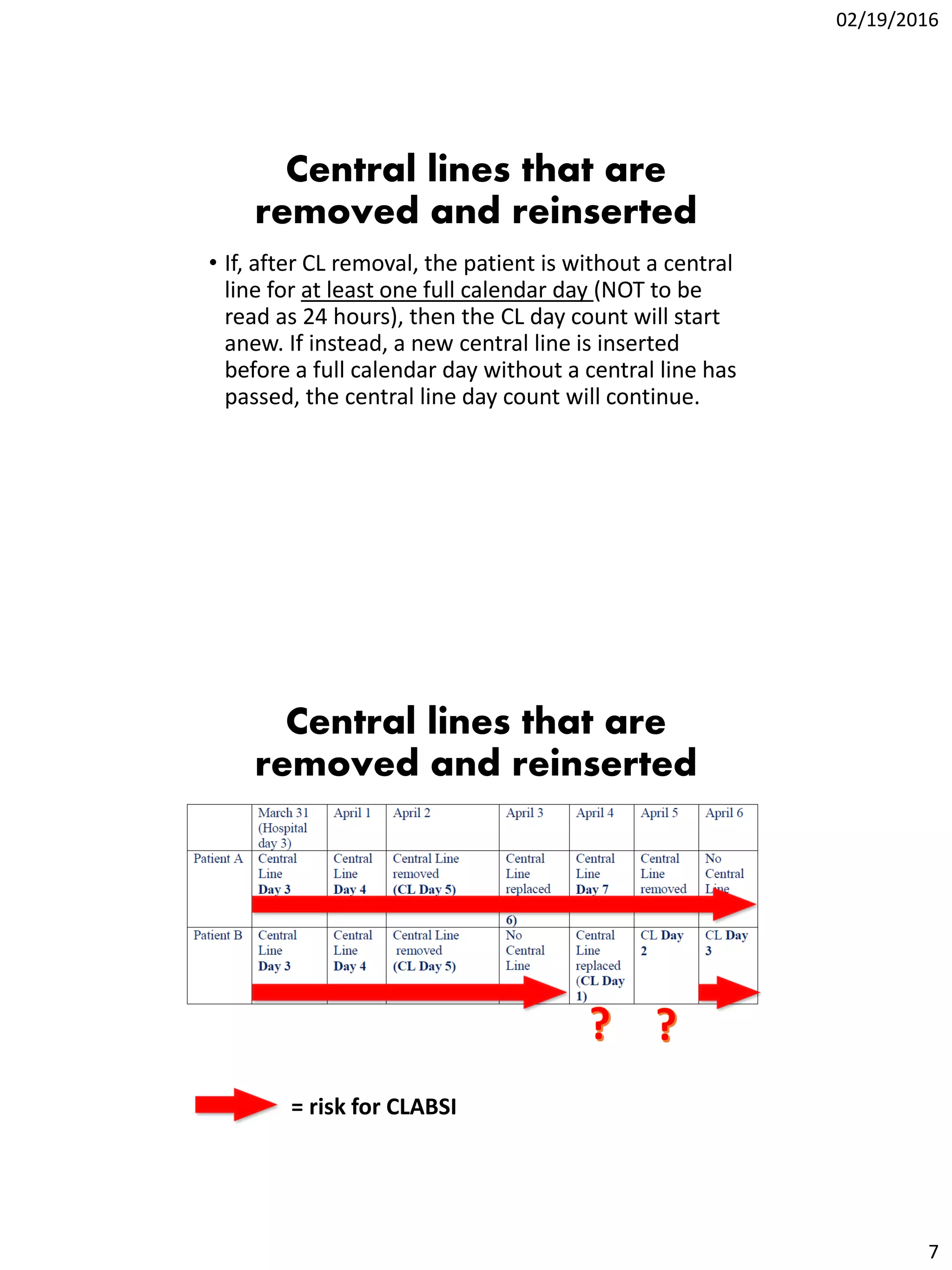
• CL in place for >2 calendar days on the date of
infection/growth, with day of device placement
being Day 1 AND the CL was in place:
oOn the date of event OR
othe day before
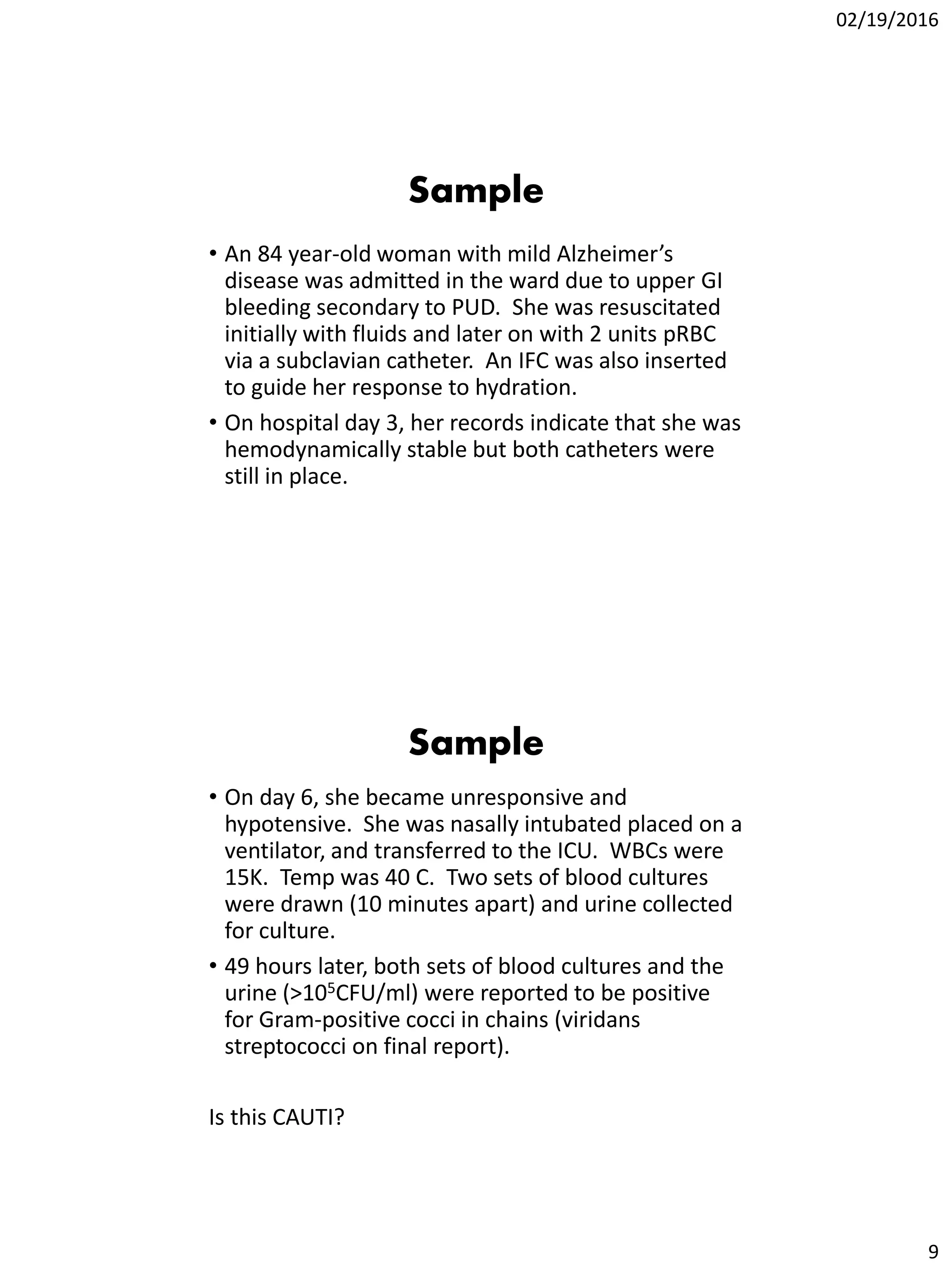
• Organism cultured from blood is not related to an
infection at another site
Same common commensal (i.e., diphtheroids
[Corynebacterium spp. not C. diphtheriae],
Bacillus spp., Propionibacterium spp., CONS,
viridans group streptococci, Aerococcus spp., and
Micrococcus spp.) is cultured from two or more
blood cultures drawn on separate occasions
Patient has a recognized
pathogen cultured from
one or more blood
cultures
1. Blood and site-specific specimen cultures match for at least one organism.
Ex: Patient with symptomatic UTI (suprapubic tenderness and >105 CFU/ml of E. coli)
and blood culture collected grows E. coli and P. aeruginosa. This is an HAI SUTI with a
secondary BSI and the reported organisms are E. coli and P. aeruginosa, since both
site and blood culture are positive for at least one matching pathogen.
2. Blood and site-specific specimen cultures do not match BUT the blood isolate
can be attributed to the distant site of infection.
Ex1: Post-op patient becomes develops fever and abdominal pain. Blood and an
aseptically-obtained T-tube drainage specimen are collected for culture. A CT scan
done that day shows fluid collection suggestive of infection. Culture results show E.
coli from the T-tube drainage specimen and blood grows Bacteroides fragilis.
Ex2: Patient has new-onset fever, cough and new infiltrates on CXR. Blood and BAL
cultures are collected. Culture results show Klebsiella pneumoniae > 104 cfu/ml from
the BAL and Pseudomonas aeruginosa from the blood.
• CL in place for >2 calendar days on the date of
infection/growth, with day of device placement
being Day 1 AND the CL was in place:
oOn the date of event OR
othe day before
• Organism cultured from blood is not related to an
infection at another site](https://image.slidesharecdn.com/haisurveillancedefinitionsandstandardizations-160308035935/75/HAI-Surveillance-Definitions-and-Standardizations-6-2048.jpg)
![02/19/2016
20
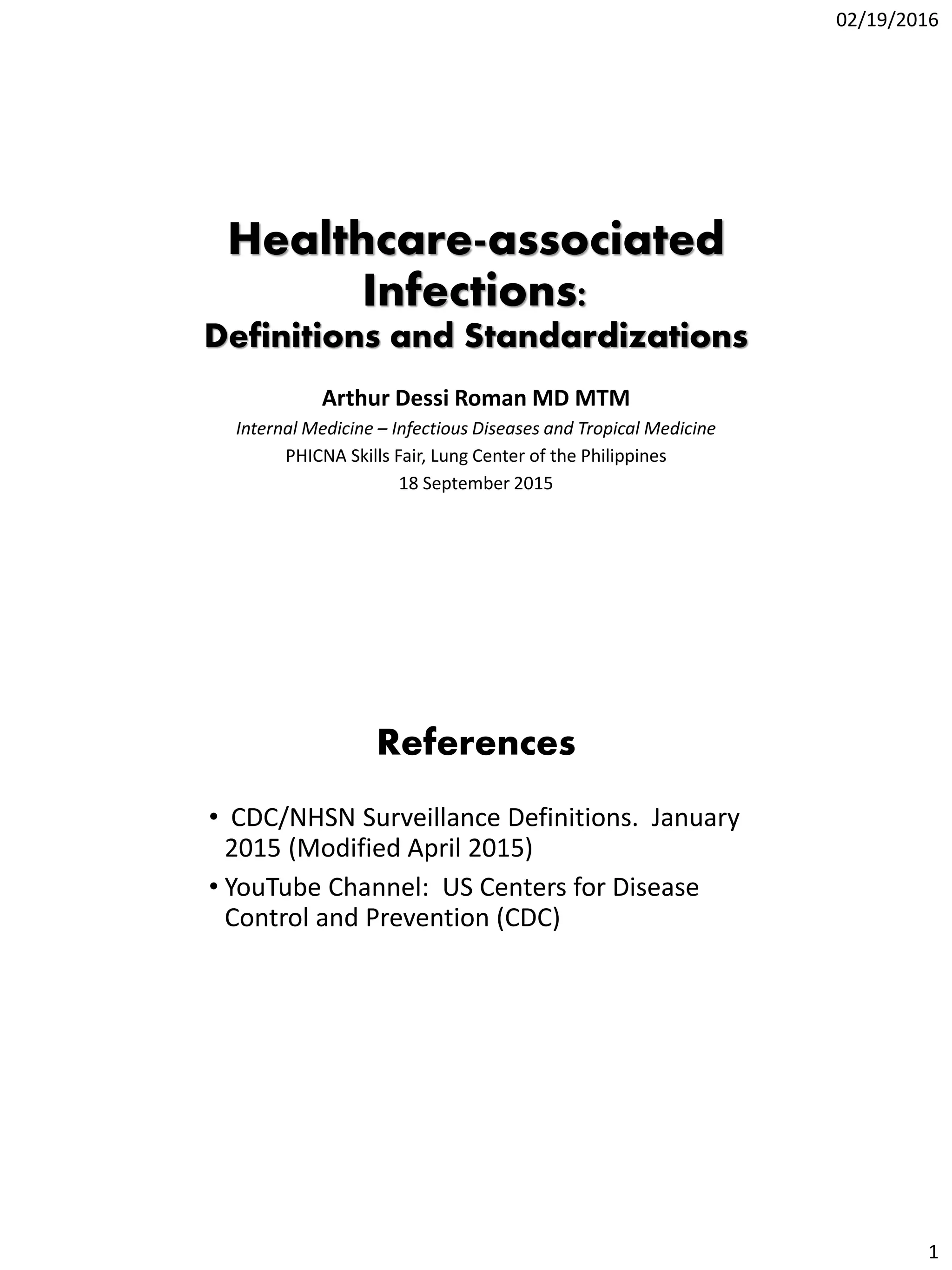
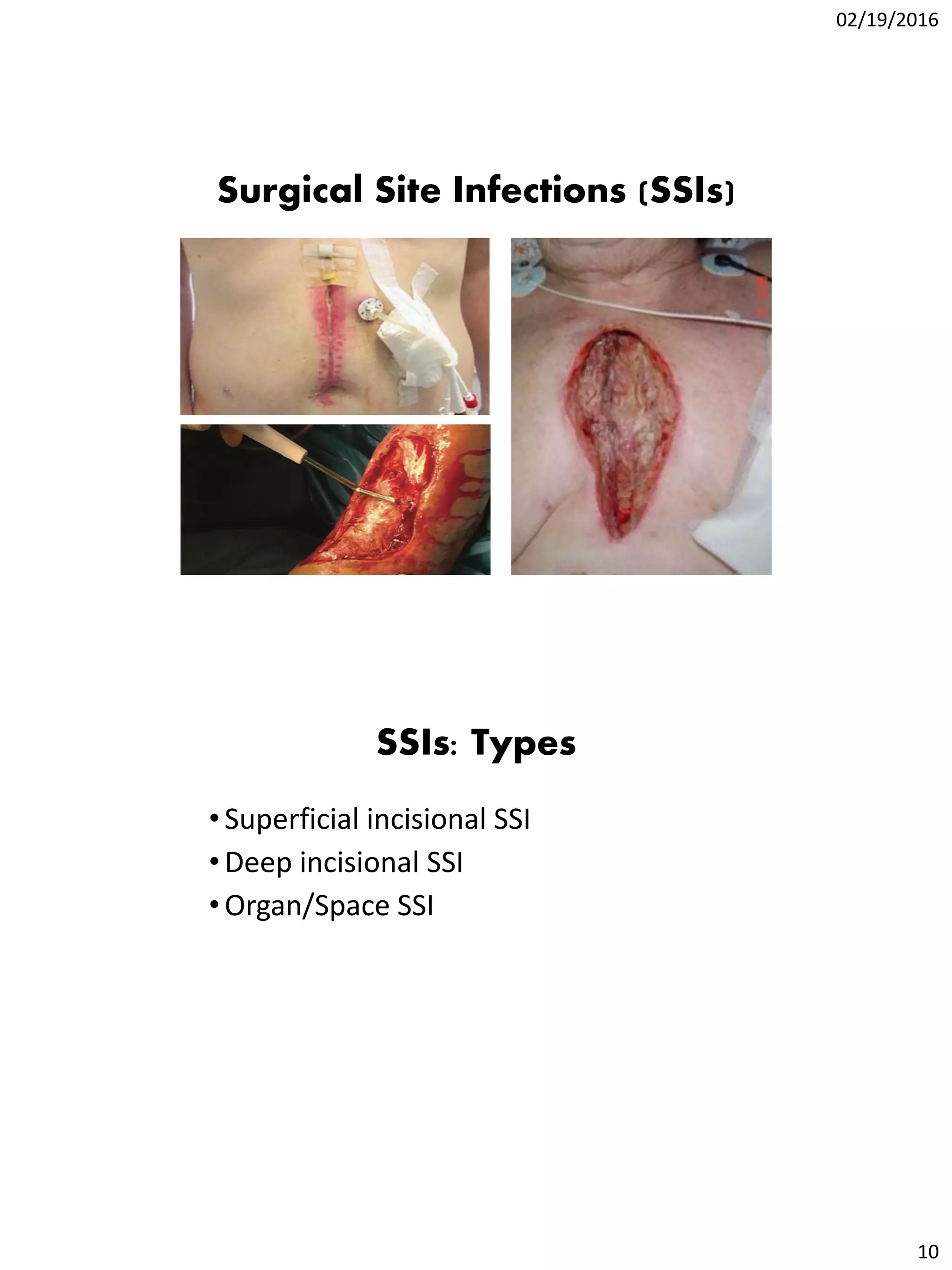
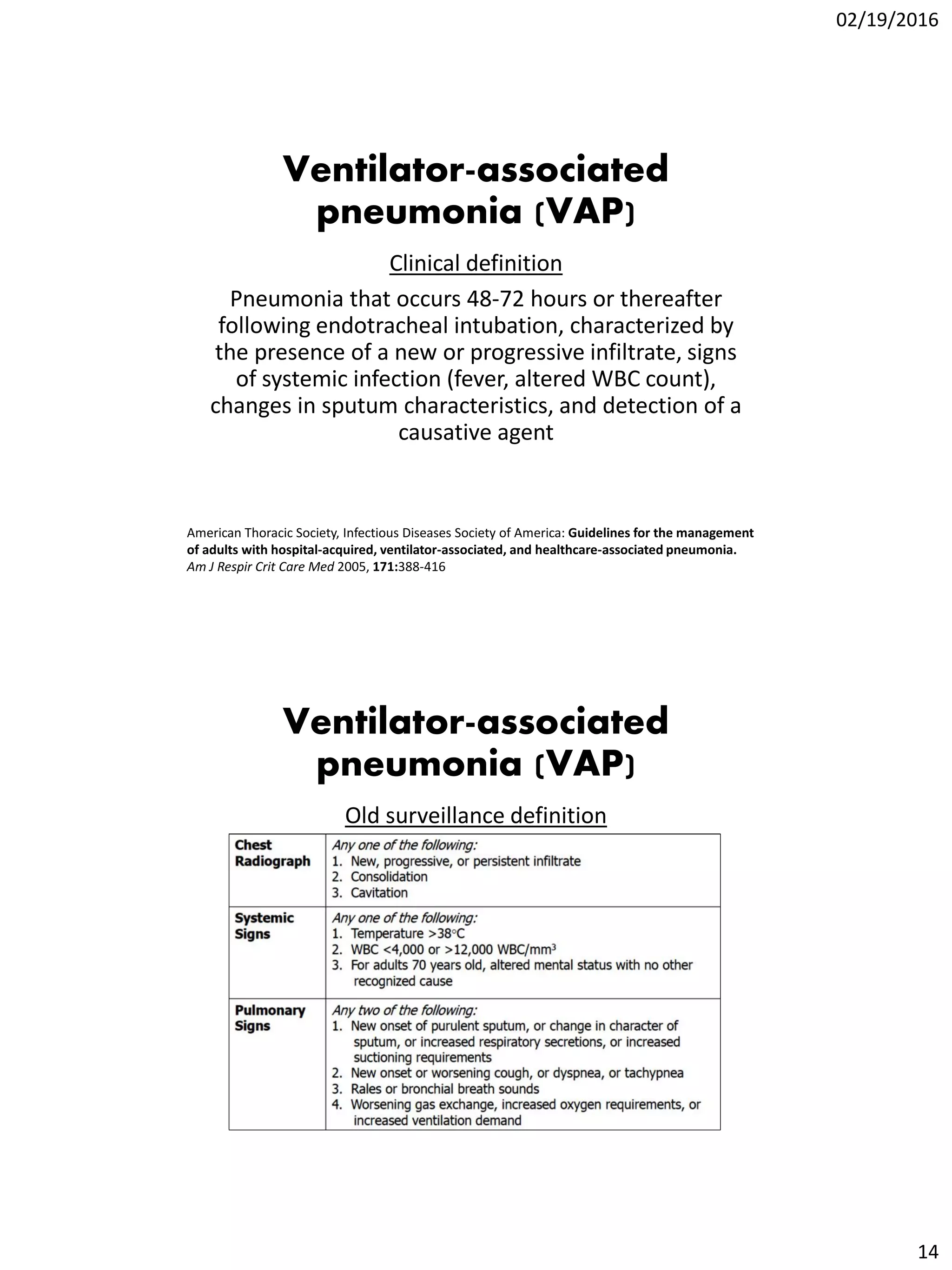
Additional Pointers
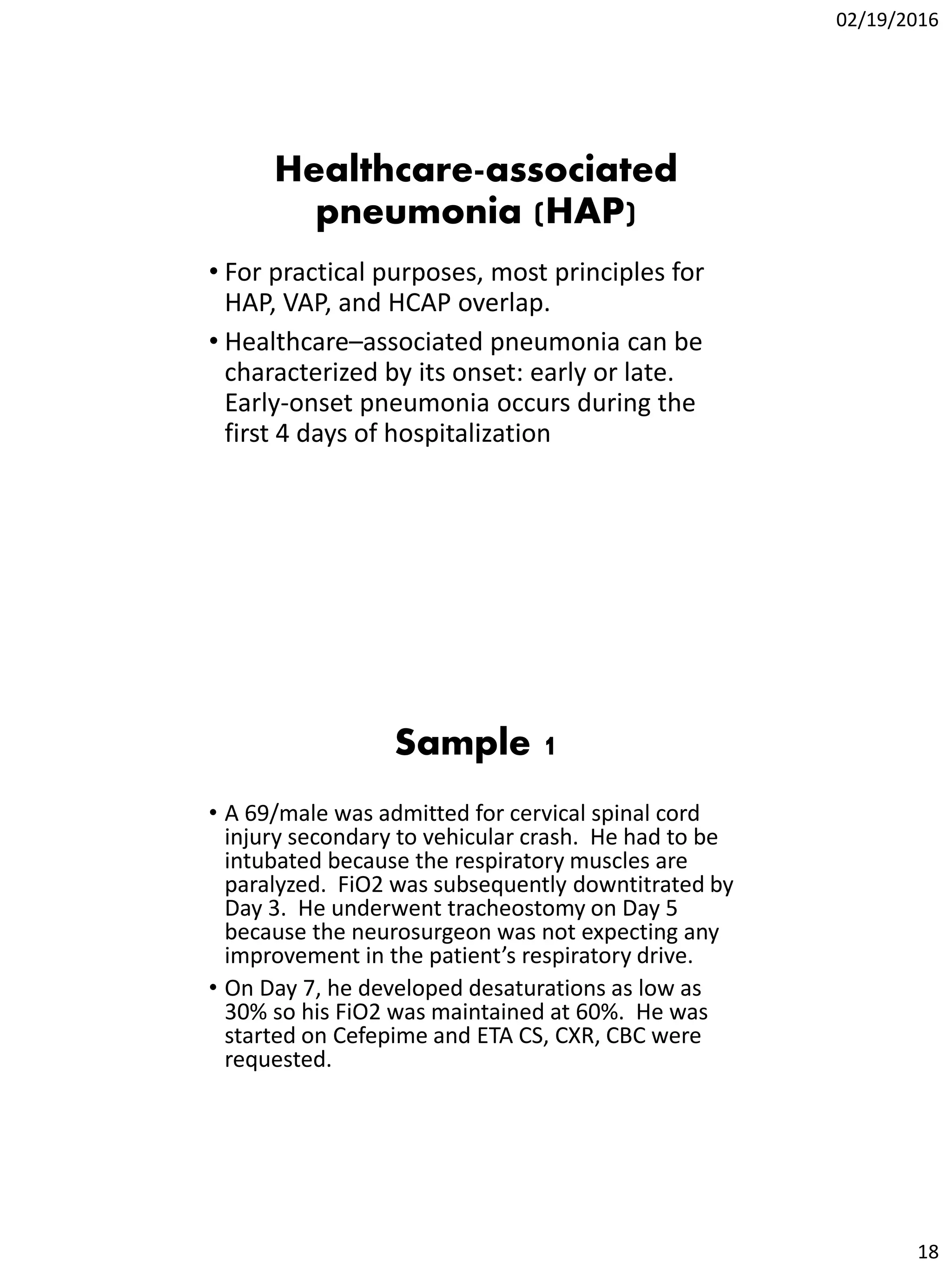
1. Provide details about your report (in the title):
• Time period
• Location
• Type of surveillance performed
“Healthcare-associated infection rates in the
[ICU/MICU/Ward] Section of [name of hospital] from
[indicate time period] generated through [type of
surveillance] surveillance conducted [frequency of
surveillance, e.g. monthly, quarterly, etc.]
Additional Pointers
2. Clinical diagnosis of HAIs may not be
consistent with the surveillance diagnosis.
In such cases, the infection control
physician shall make the final call if the
case is an HAI or not.](https://image.slidesharecdn.com/haisurveillancedefinitionsandstandardizations-160308035935/75/HAI-Surveillance-Definitions-and-Standardizations-20-2048.jpg)