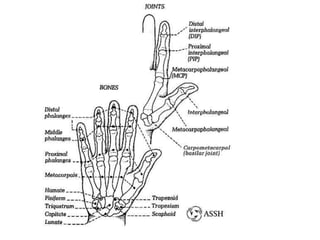
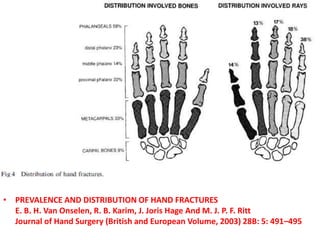
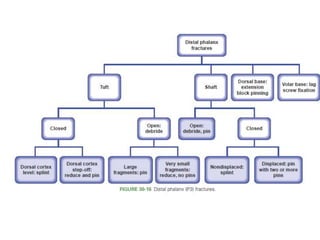
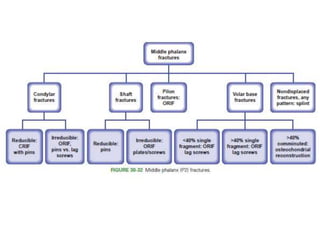
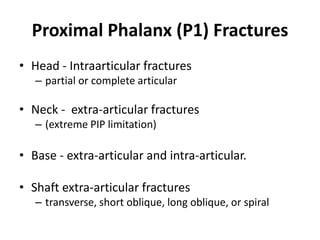
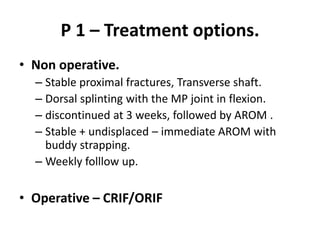
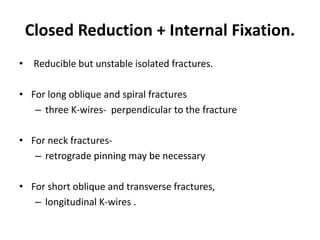
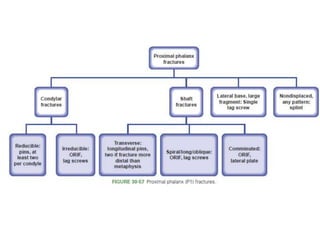
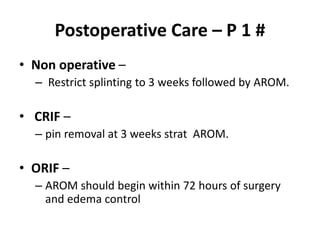
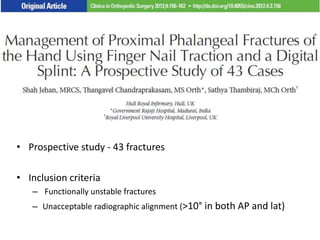
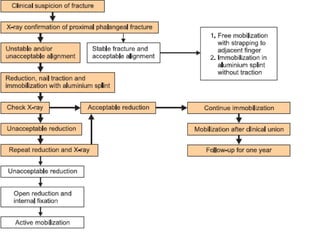
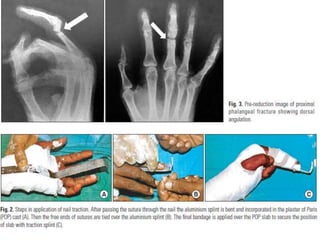
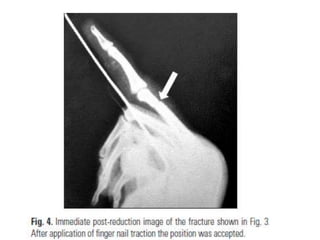
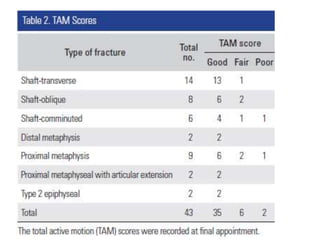
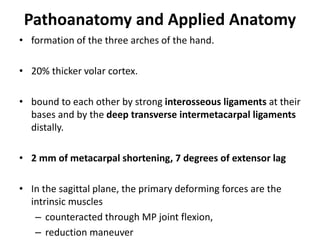
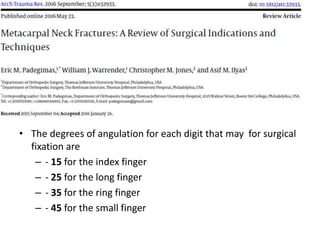
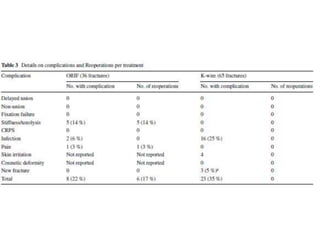
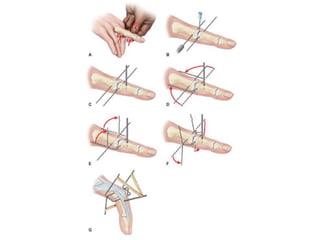
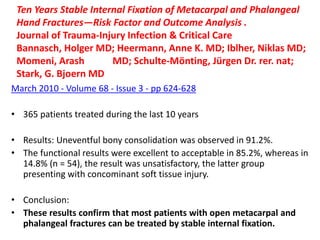
This document summarizes principles for the management of hand fractures presented by Dr. REJUL K RAJ. It discusses anatomy of the hand bones, common fracture patterns, mechanisms of injury, signs and symptoms, imaging, classification systems, treatment principles including splinting and various operative fixation methods, and postoperative care. Key points covered include fracture patterns of the distal phalanx, middle phalanx, proximal phalanx and metacarpals as well as treatment approaches for each. Studies on outcomes of K-wire fixation versus ORIF for metacarpal fractures are summarized.






































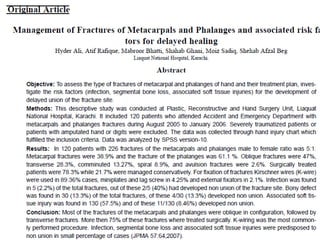

![• Journal of Trauma-Injury Infection & Critical Care:
• March 2002 - Volume 52 - Issue 3 - pp 535-539
• Original Articles
• Complications of Plate Fixation in Metacarpal Fractures
• Fusetti, Cesare MD; Meyer, Henning MD; Borisch, Nicola MD; Stern, Richard MD; Santa, Dominique
Della MD; Papaloïzos, Michael MD
• Abstract
• Background : The objective of this study is to assess the complications after open reduction and
plate fixation of extra-articular metacarpal fractures.
• Methods : We retrospectively reviewed the clinical and radiologic records of 129 consecutive
patients with 157 metacarpal fractures treated by open reduction and internal fixation with plates
between 1993 and 1999. Intra-articular fractures and fractures of the thumb metacarpal were
excluded. Eighty-one patients (64 men and 17 women) with 104 fractures were available for
review, at an average follow-up of 13.6 months (range, 6–27 months).
• Results : Twenty-eight patients (35%) and 33 fractures (32%) had one or more complications,
including difficulty with fracture healing (12 patients [15%]), stiffness (eight patients [10%]), plate
loosening or breakage (seven patients [8%]), complex regional pain syndrome (two patients), and
one patient who developed a deep infection.
• Conclusion : Despite technical advances in implant material, design, and instrumentation, plate
fixation of metacarpal fractures remains fraught with complications and unsatisfactory results.](https://image.slidesharecdn.com/rejulhandfractures-180515094247/85/Hand-fracture-Management_Rejul-155-320.jpg)