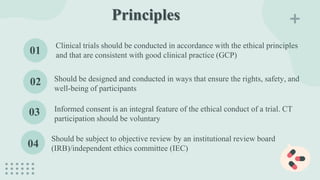
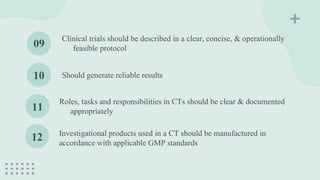
Good Clinical Practice (GCP) is an international ethical and scientific standard ensuring the integrity of clinical trials involving human participants, covering everything from trial design to data analysis, with a strong focus on participant rights and safety. Originating from key historical documents, GCP guidelines have evolved to include detailed principles and responsibilities for investigators, sponsors, and ethics committees. The ICH GCP E6 guidelines, essential for all stakeholders in clinical research, emphasize the importance of informed consent, scientific validity, and compliance with ethical standards to protect participants and enhance the reliability of trial results.