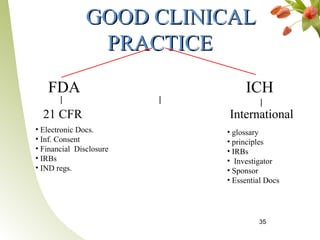
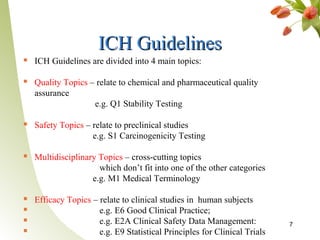
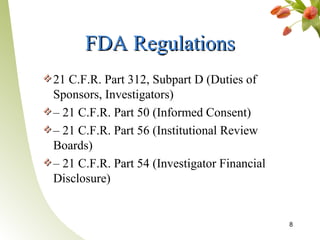
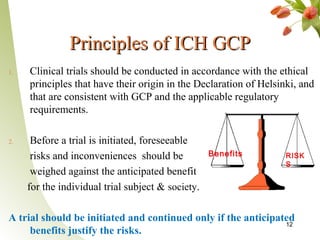
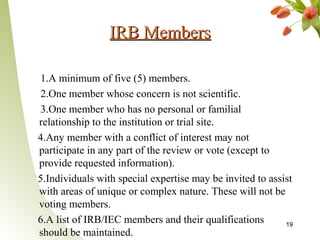
Good Clinical Practice (GCP) provides quality standards for clinical research to ensure human subjects are protected and study results are reliable. Key responsibilities include Institutional Review Boards overseeing studies, investigators providing medical care and adhering to protocols, and sponsors manufacturing products and monitoring trials. GCP aims to conduct ethical research through informed consent, qualifications of researchers, and quality management systems.