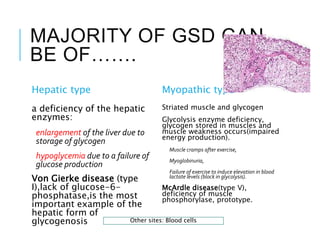
Glycogen storage diseases are a group of inherited metabolic disorders caused by deficiencies of enzymes involved in glycogen breakdown or synthesis. This leads to abnormal glycogen buildup in tissues. The main types are GSD I, III and IV. In GSD I, glucose-6-phosphatase is deficient causing hypoglycemia and liver enlargement. GSD III results from a debranching enzyme defect causing abnormal glycogen structure. GSD IV involves branching enzyme deficiency and liver cirrhosis. Symptoms vary by type but may include low blood sugar, enlarged liver, muscle cramps and failure to thrive. Treatment focuses on a high-carbohydrate diet and cornstarch to manage blood sugar levels. Prognosis depends on
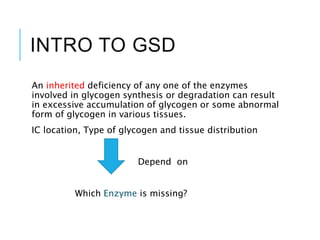
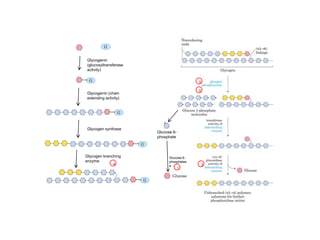
![Number
Enzyme
deficiency
Eponym Incidence
Hypo-
glycemia?
Hepato-
megaly?
Hyperlip-
idemia?
Muscle
symptoms
Development/
prognosis
Other
symptoms
GSD type 0
glycogen
synthase
- Yes No No
Occasional
muscle
cramping
Growth failure
in some cases
GSD type I
glucose-6-
phosphatase
von Gierke's
disease
1 in 50,000
100,000[
births
Yes Yes Yes None Growth failure
Lactic
acidosis,
hyperuricem
ia
GSD type II
acid alpha-
glucosidase
Pompe's
disease
1 in 40,000
births-50,000
No Yes No
Muscle
weakness
*Death by age
~2 years
(infantile
variant)
heart failure
GSD type III
glycogen
debranching
enzyme
Cori's disease
or Forbes'
disease
1 in 100,000
births
Yes Yes Yes Myopathy
GSD type IV
glycogen
branching
enzyme
Andersen
disease
1 to 500,000 No
Yes,
also
cirrhosis
No None
Failure to
thrive, death
at age ~5
years
GSD type V
muscle
glycogen
phosphorylas
e
McArdle
disease
1 in 100,000-
500,000
No No No
Exercise-
induced
cramps,
Rhabdomyoly
sis
Renal failure
by
myoglobinur
ia, second
wind
phenomeno
n
GSD type VI
liver glycogen
phosphorylas
e
Hers' disease
1 in 65,000-
85,000 births] Yes Yes Yes [15] None
initially
benign,
growth
retardation
follows.
GSD type VII
muscle
phosphofruct
okinase
Tarui's
disease
1 in
1,000,000
No No No
Exercise-
induced
muscle
cramps and
weakness
growth
retardation
Haemolytic
anaemia
GSD type IX
Phosphorylase
kinase
Yes Yes Yes None
Delayed
motor
development,
Growth
retardation](https://image.slidesharecdn.com/glycogenstoragedisease-170317210117/85/Glycogen-storage-disease-LB-12-320.jpg)