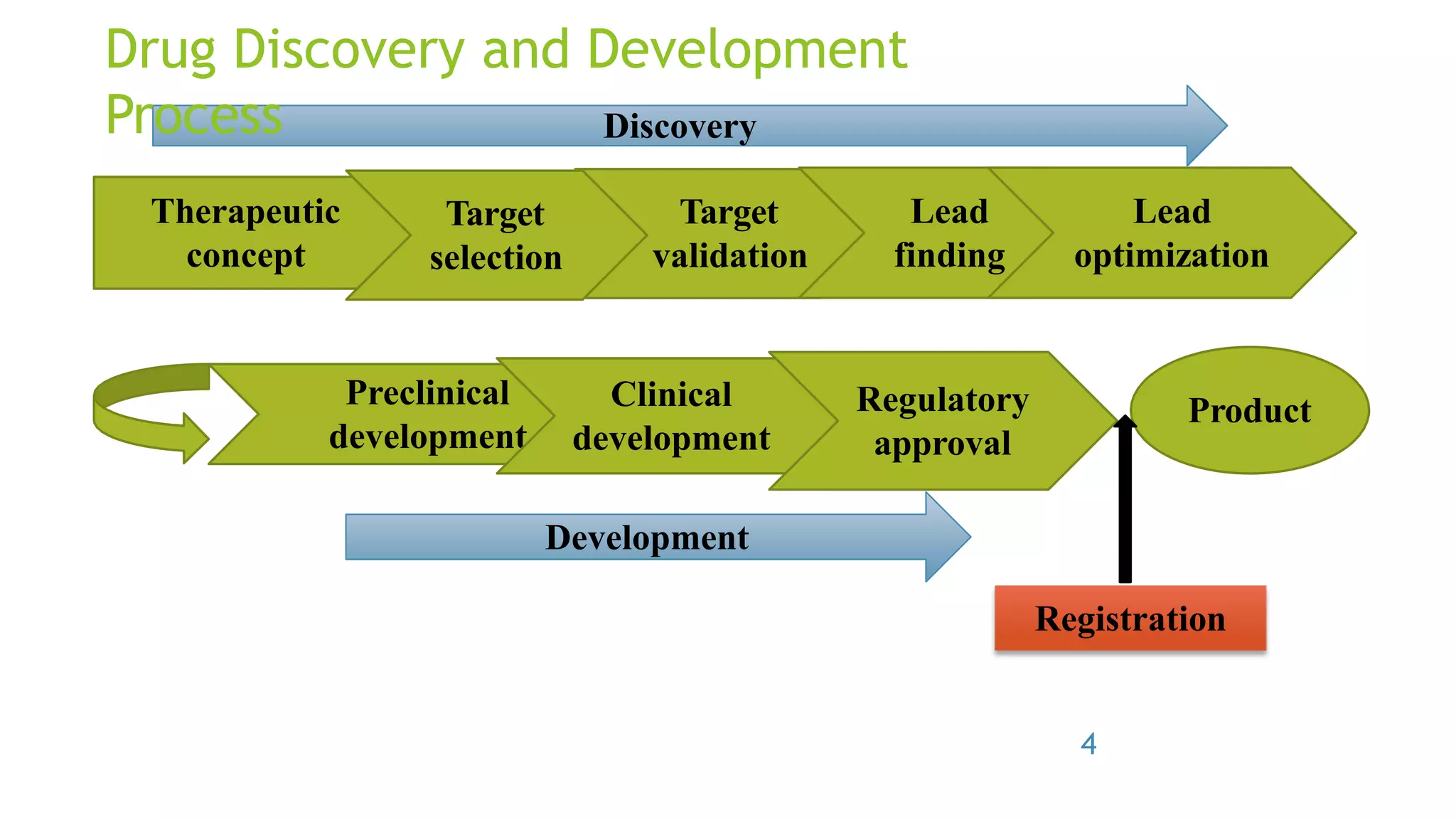
The document provides an introduction to Good Laboratory Practice (GLP). It discusses how in the 1970s, the FDA discovered many cases of poor laboratory practices and fraudulent activities in the US. This led to the formal creation of GLP regulations by the FDA and OECD to ensure quality and reliability in non-clinical safety studies. The key principles of GLP include standardized operations in areas like facilities, equipment, test systems, protocols, record-keeping and reporting to ensure study data accurately represent results. Compliance with GLP aims to produce high-quality data and gain mutual acceptance of studies internationally.