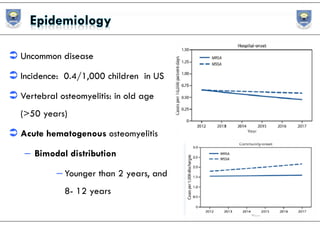
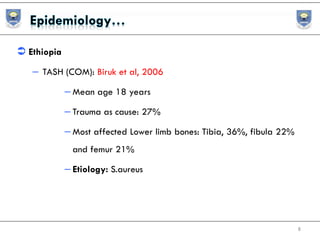
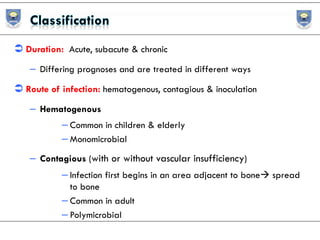
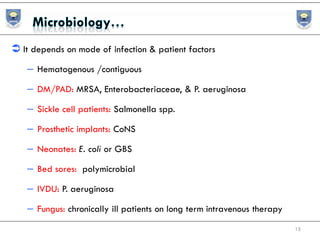
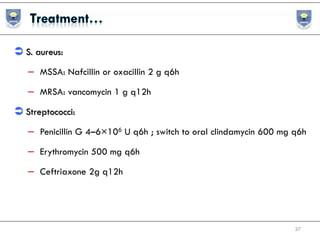
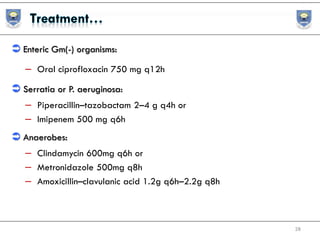
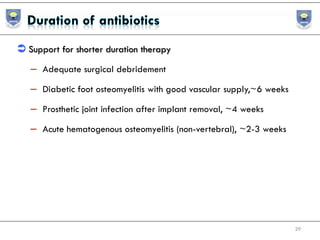
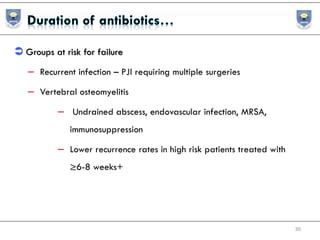
Osteomyelitis is a severe bone infection that can be acute or chronic, with Staphylococcus aureus being the most common cause. Treatment involves antibiotics combined with surgical debridement or drainage of abscesses. The goals of treatment are to eradicate the infection, resolve symptoms, and prevent complications through a multi-disciplinary approach and prolonged antibiotic therapy.