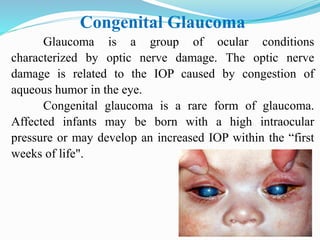
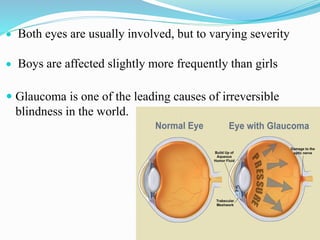
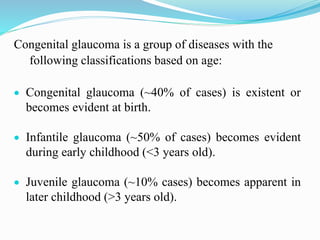
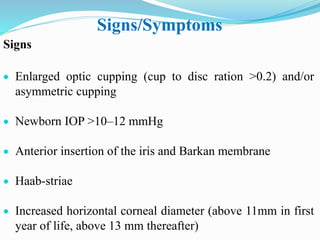
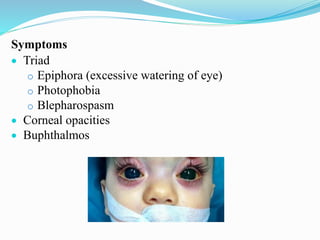
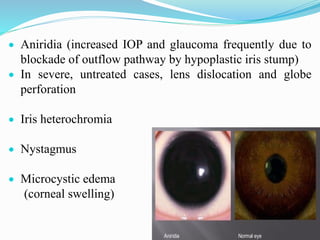
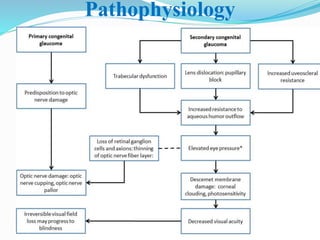
Congenital glaucoma is a group of rare ocular conditions characterized by optic nerve damage due to high intraocular pressure, often evident at birth or in early childhood, and is a leading cause of irreversible blindness. Diagnosis requires a thorough examination under anesthesia, with management options including medical treatments like beta-blockers and surgical procedures such as goniotomy and trabeculectomy. Nursing management emphasizes monitoring, education for parents, and strict aseptic techniques during care.