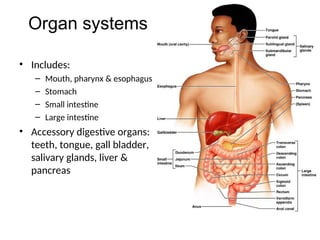
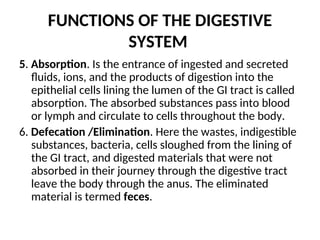
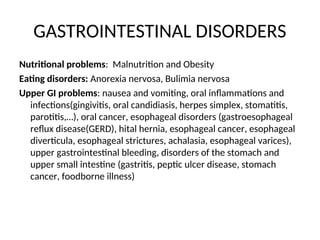
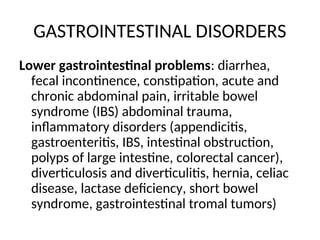
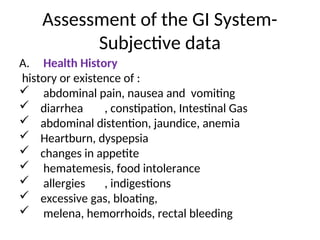
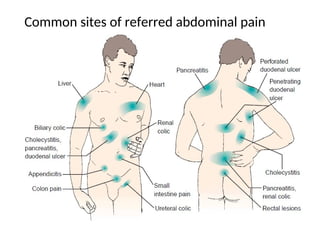
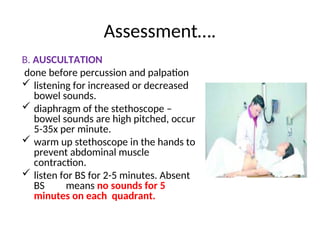
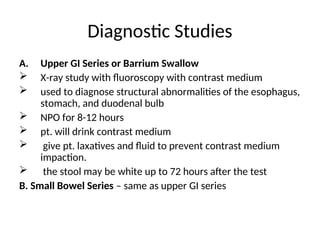
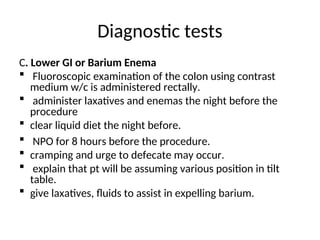
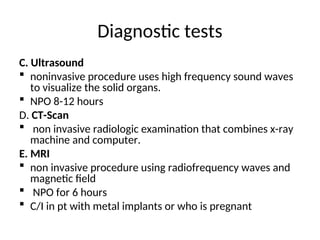
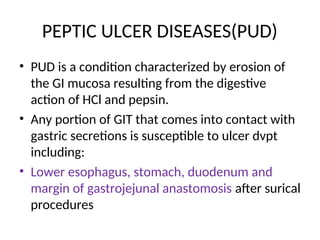
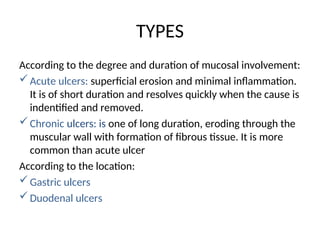
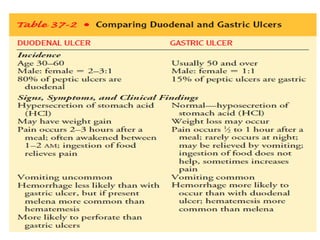
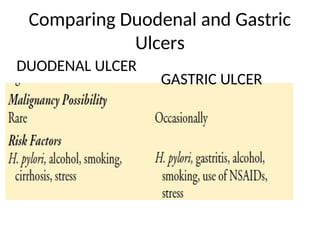
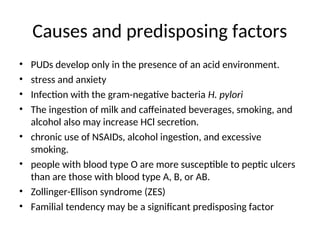
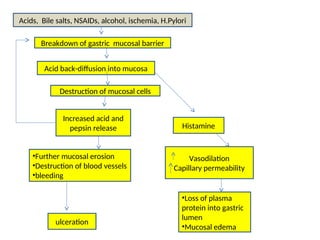
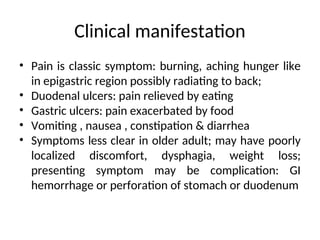
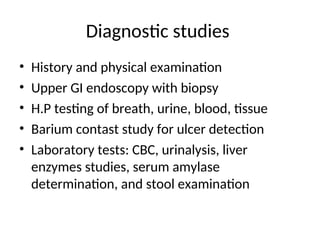
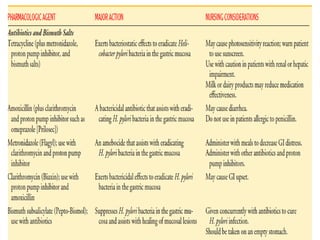
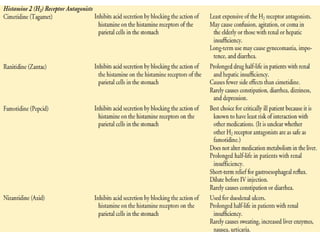
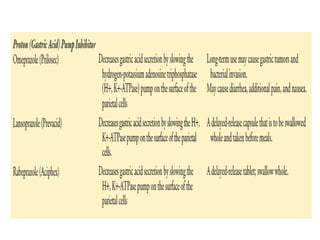
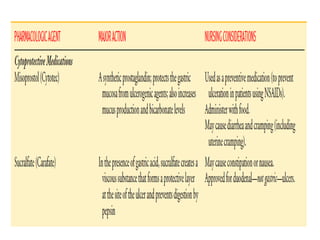
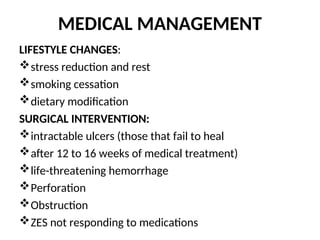
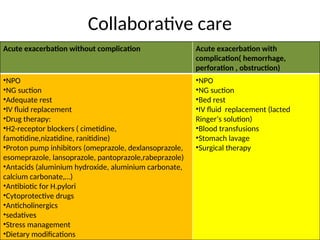
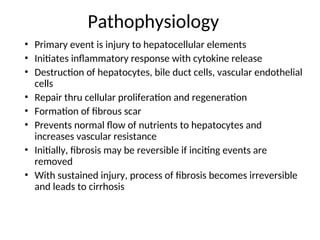
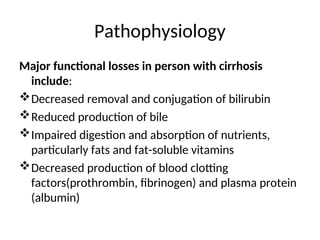
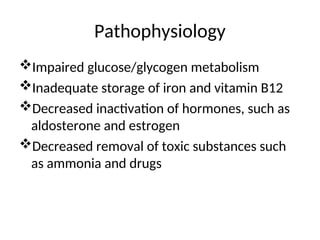
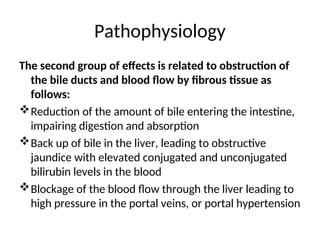
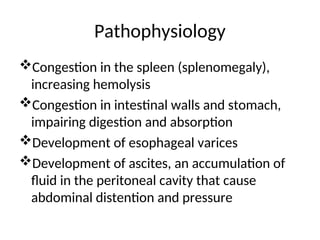
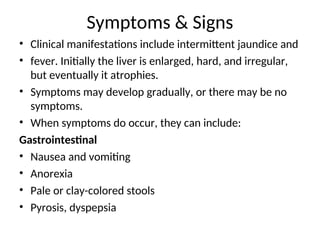
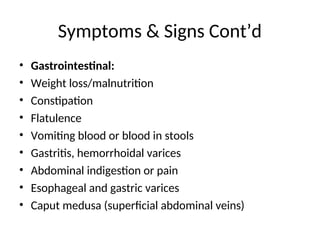
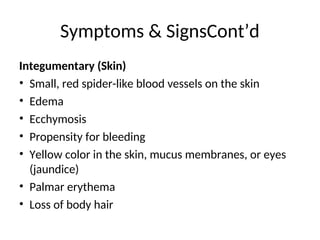
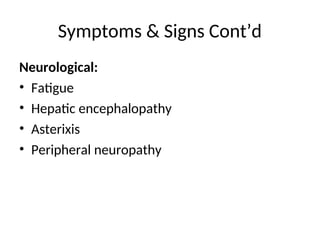
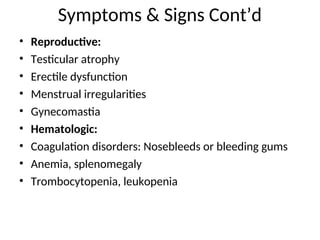
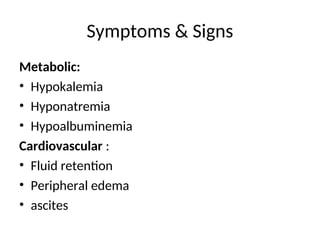
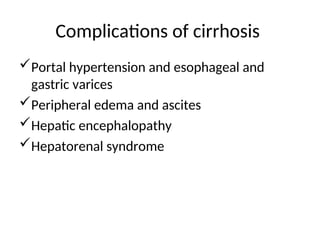
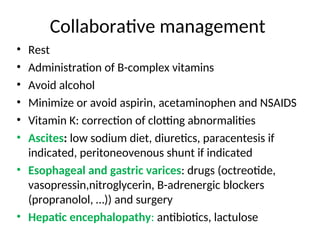
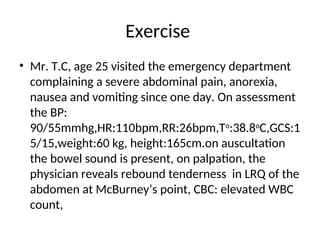
The document covers the gastrointestinal (GI) system, detailing its structure, functions, and common disorders, including upper and lower GI problems, as well as liver and pancreatic disorders. It emphasizes assessment techniques such as health history, physical examination, diagnostic tests, and outlines conditions such as peptic ulcer disease and cirrhosis along with their causes, pathophysiology, and clinical manifestations. It concludes by discussing medical management and collaborative care for patients with GI disorders.