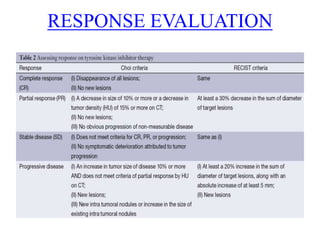
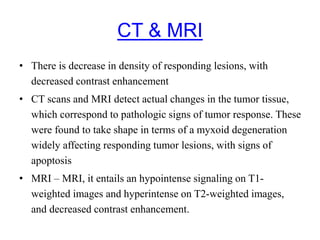
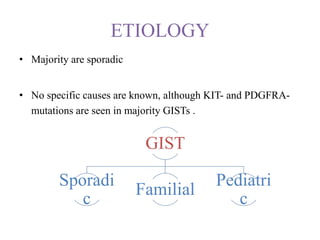
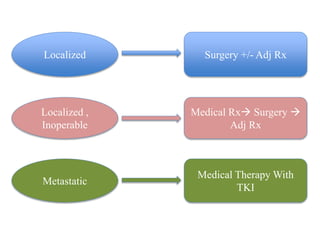
This document provides information on gastrointestinal stromal tumors (GISTs) including their definition, epidemiology, etiology, molecular pathogenesis, genetic classification, anatomy, pathology, screening, diagnosis, staging, prognostic factors, risk stratification, management of localized, advanced, inoperable, and metastatic disease, treatment with tyrosine kinase inhibitors, response evaluation, and follow up. GISTs are rare mesenchymal tumors of the GI tract that are driven by mutations in KIT or PDGFRA genes. Surgery is the main treatment for localized disease while advanced disease is treated with tyrosine kinase inhibitors.
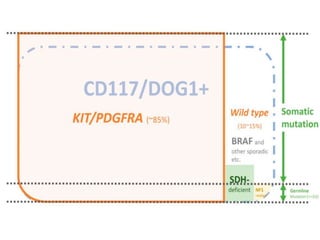
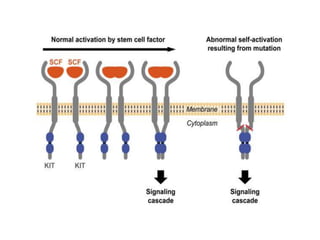
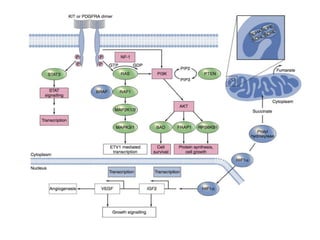
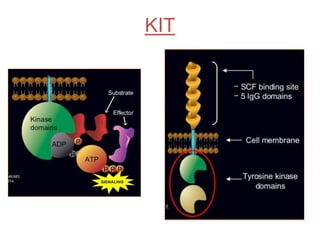
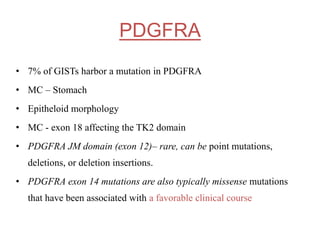
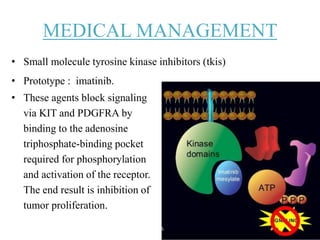
![• They are mutually exclusive and result in the constitutive
activation of either KIT or PDGFRA, which normally are
autoinhibited, being activated by the binding of their
respective ligands (i.e., stem-cell factor [Steel factor] and
platelet-derived growth factor A)
• The activation of the receptor binds two molecules of KIT or
PDGFRA (dimerization), giving rise to downstream oncogenic
signaling, which for both KIT and PDGFRA involves the
RAS/MAPK and the PI3K/AKT/mammalian target of
rapamycin (mTOR) pathways.](https://image.slidesharecdn.com/gistmine-210518064844/85/Gist-12-320.jpg)

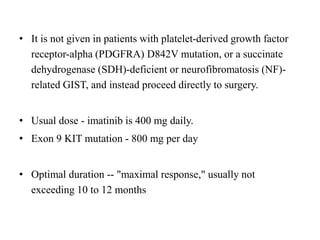
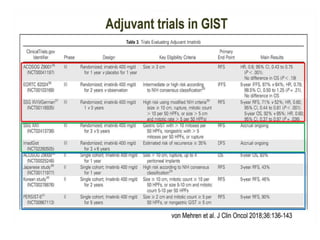
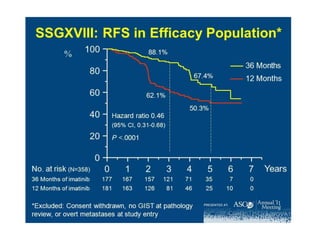
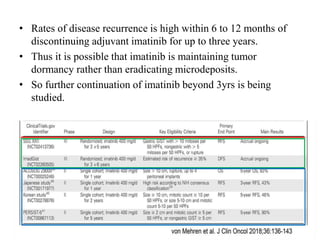
![Imatinib Duration ??
• SSG XVIII trial — The Scandinavian Sarcoma Group (SSG)
XVIII trial
• compared 36 versus 12 months of adjuvant imatinib (400 mg
daily) in 400 patients with high-risk resected GIST [23]. High-
risk was defined according to the modified consensus criteria
[24] as having at least one of the following: tumor size >10
cm, mitotic count >10 per 50 high-power fields (HPF), tumor
size >5 cm with mitotic rate >5/HPF, or tumor rupture.](https://image.slidesharecdn.com/gistmine-210518064844/85/Gist-68-320.jpg)