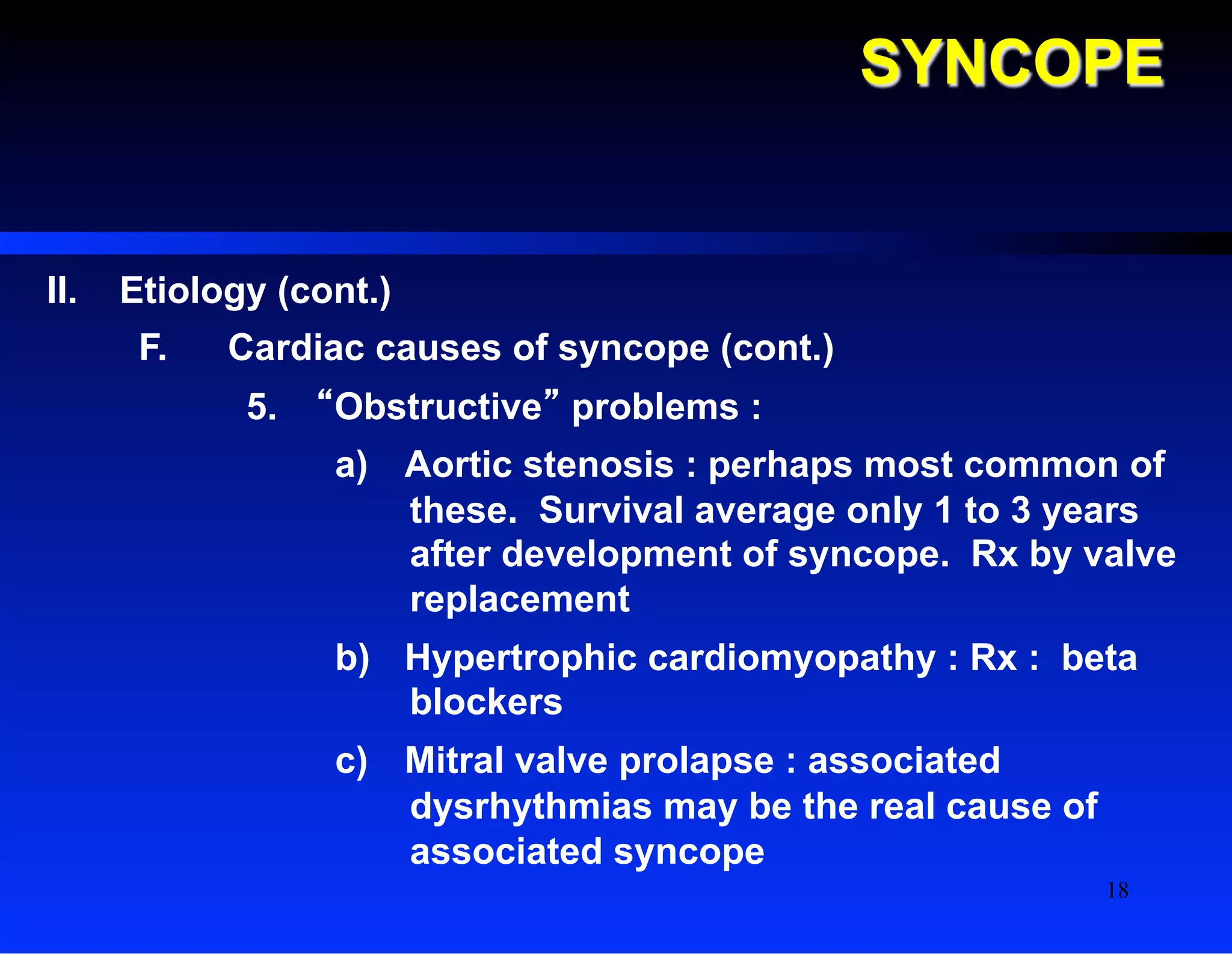
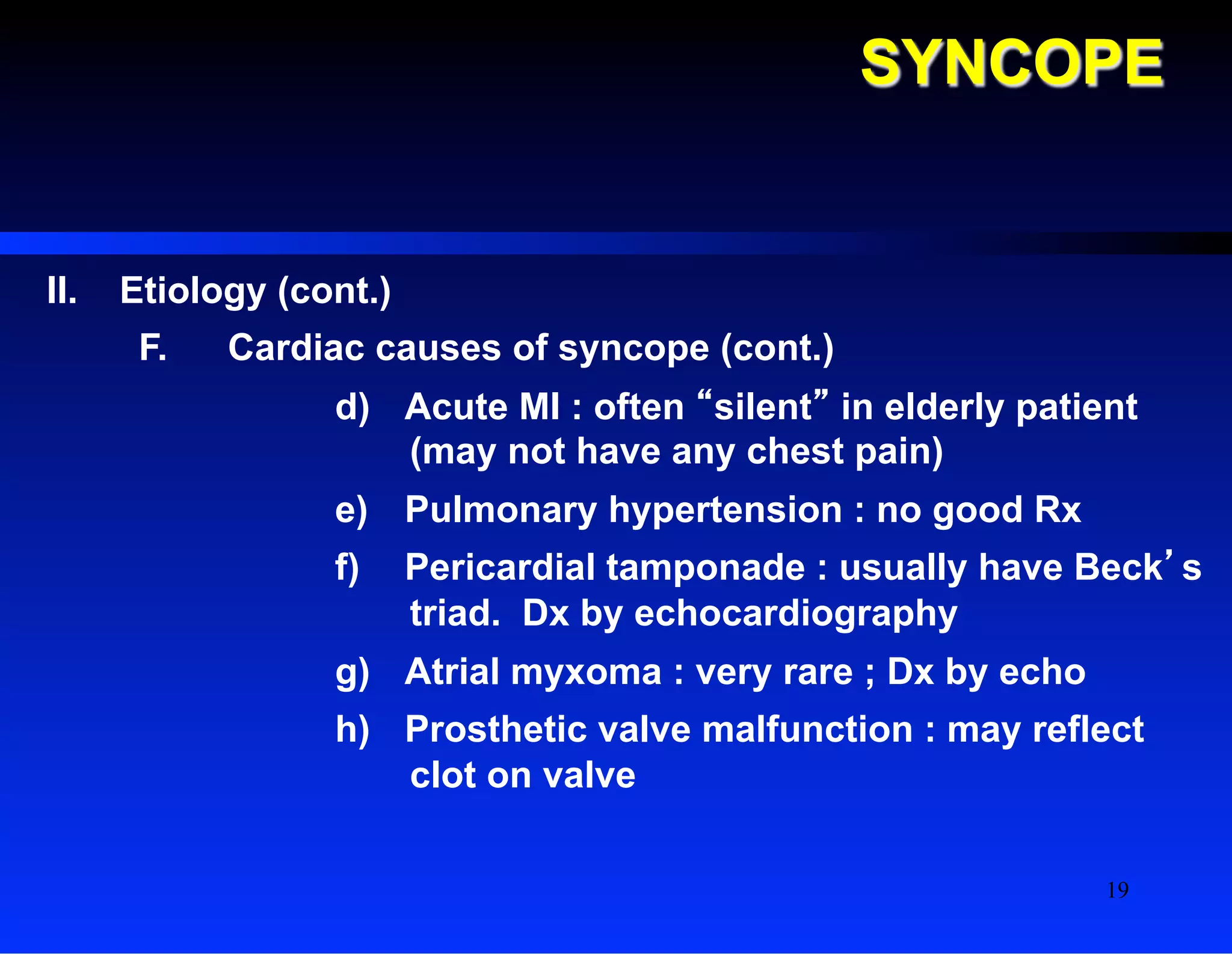
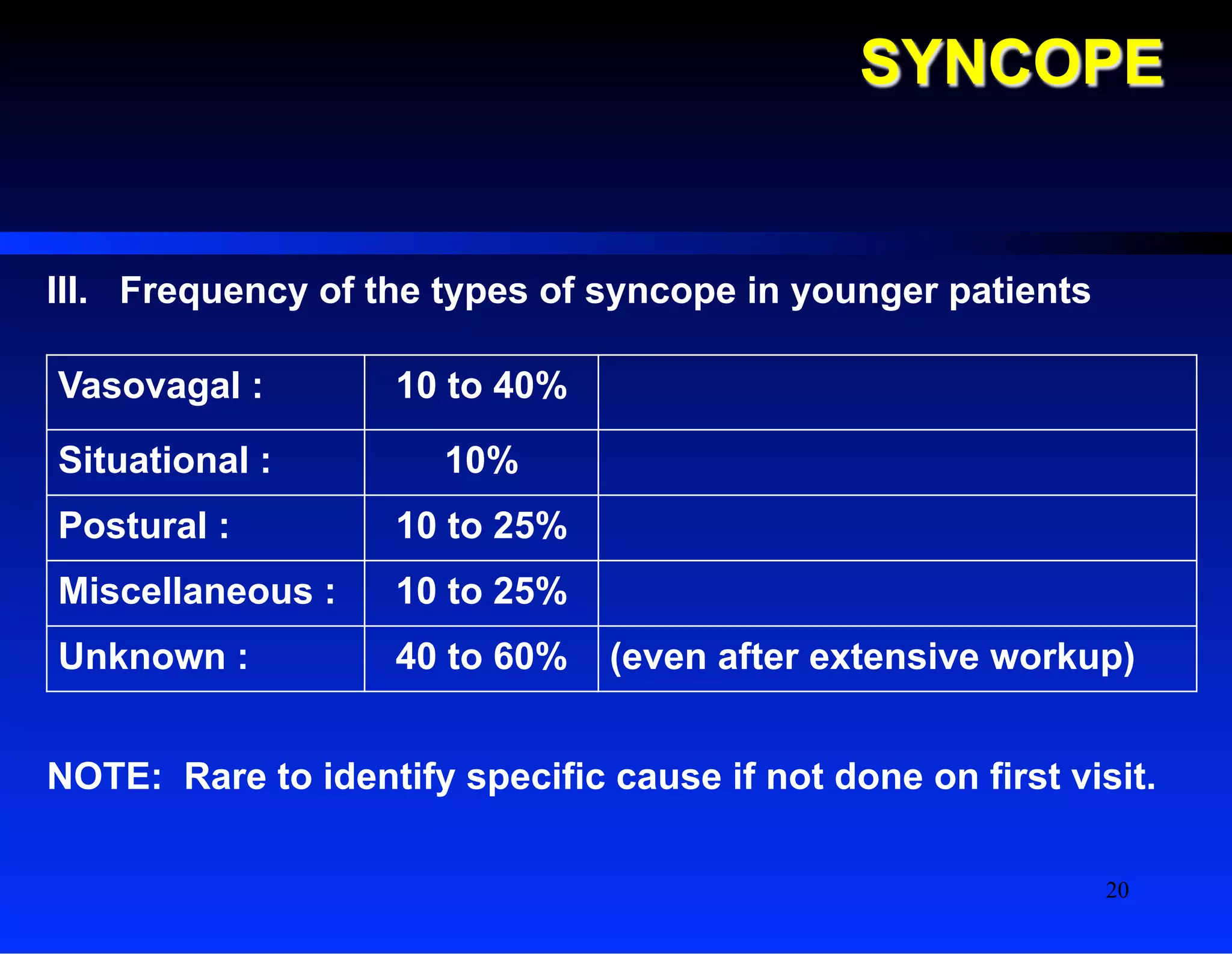
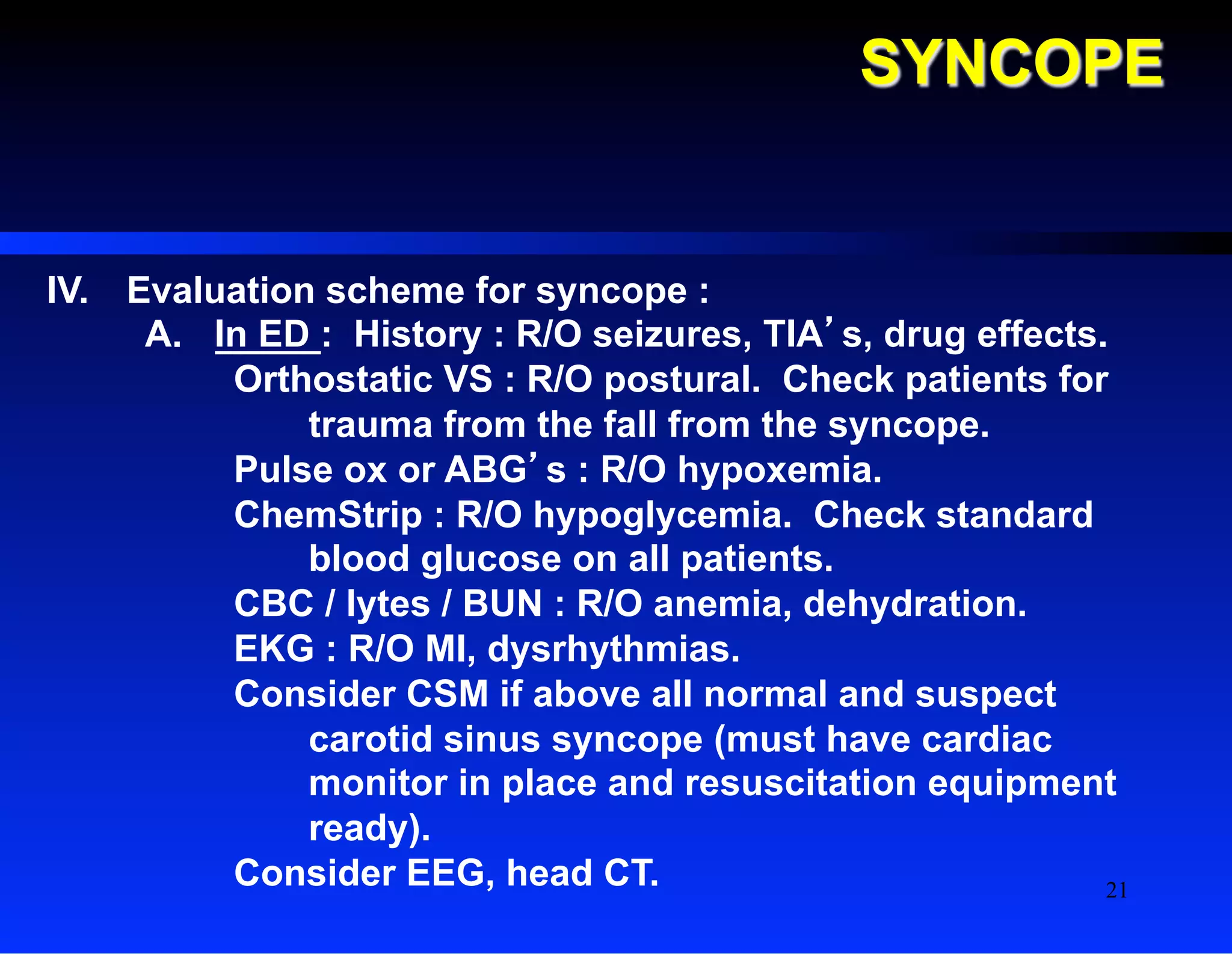
The document discusses syncope, defined as a sudden temporary loss of consciousness associated with loss of postural tone, and outlines various etiologies including vasovagal, situational, and cardiac causes. It emphasizes the importance of proper evaluation and management depending on the suspected cause, while also informing that medical content should not be used for self-diagnosis. Additionally, it provides guidelines for treatment and recommendations for further testing in specific cases.