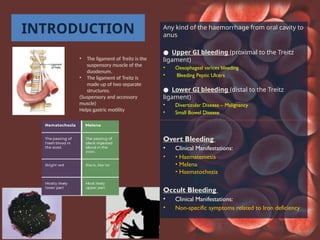
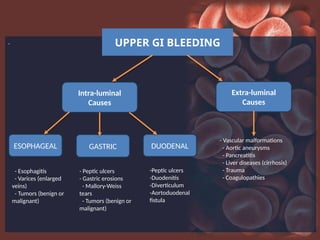
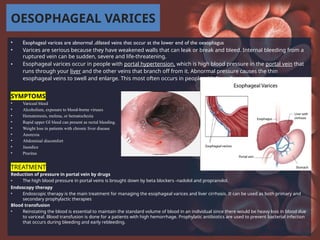
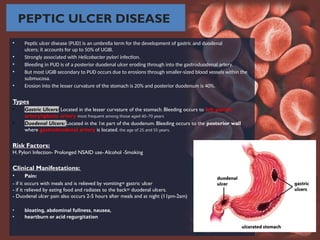
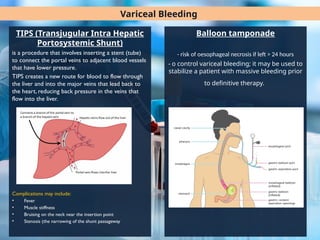
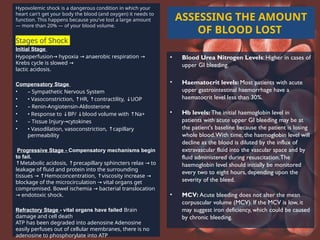
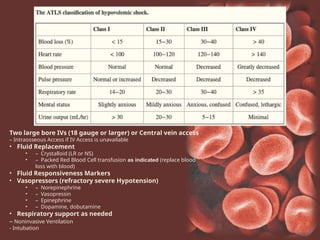
This document discusses gastrointestinal bleeding, categorizing it into upper and lower GI bleeding, along with their causes, clinical manifestations, and treatments. It emphasizes the importance of diagnosing conditions like peptic ulcers, esophageal varices, and erosive gastritis, highlighting both pharmacological and endoscopic interventions. Additionally, it outlines the diagnostic procedures, management strategies, and complications associated with these types of bleeding.