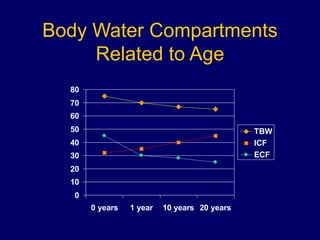
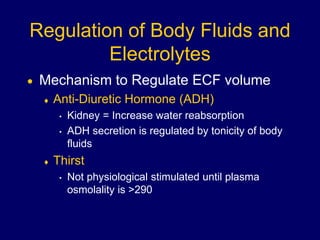
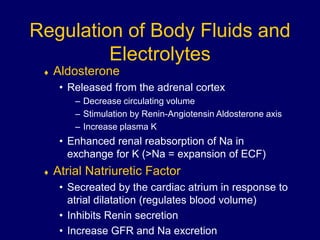
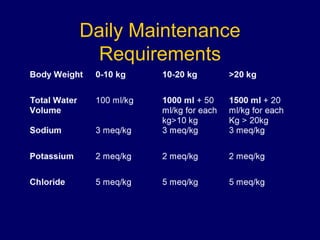
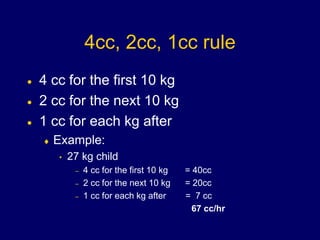
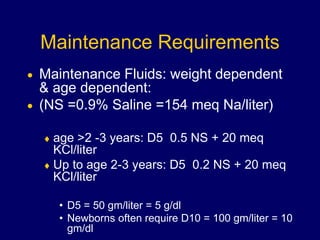
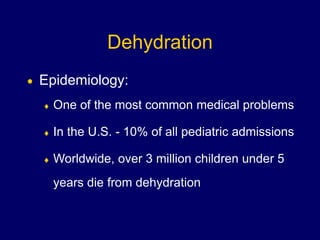
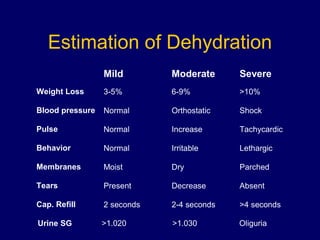
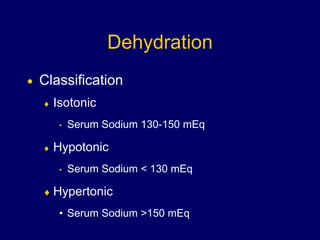
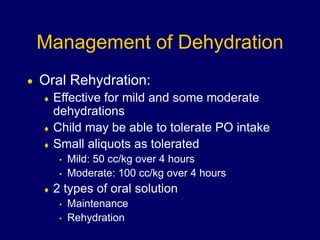
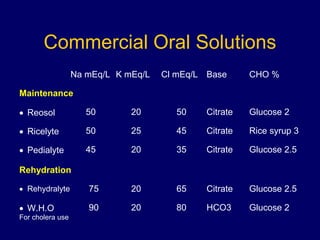
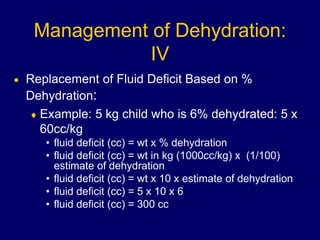
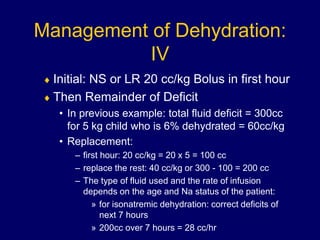
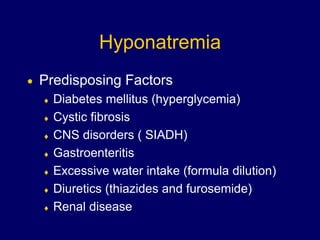
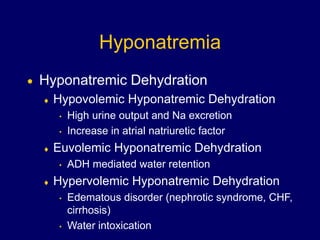
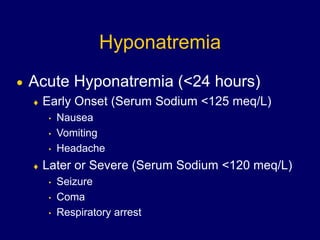
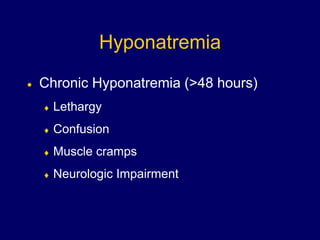
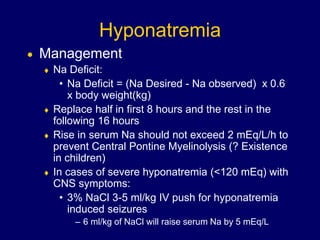
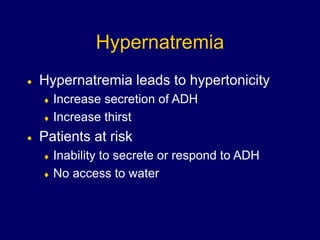
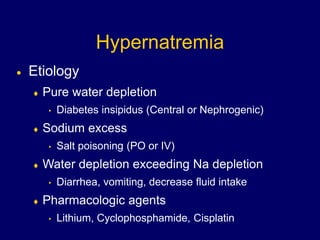
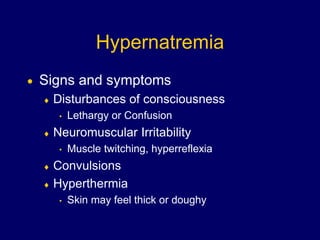
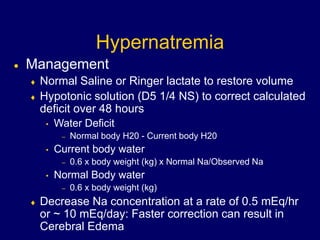
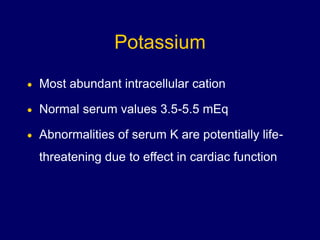
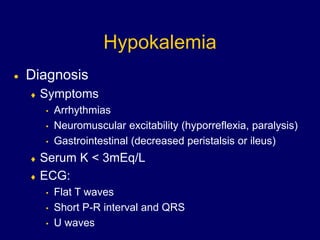
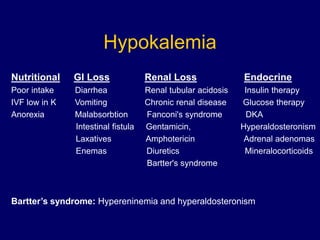
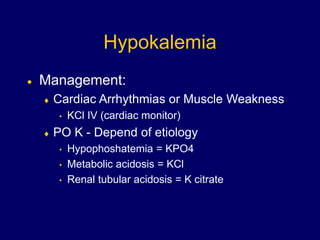
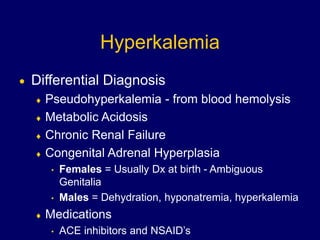
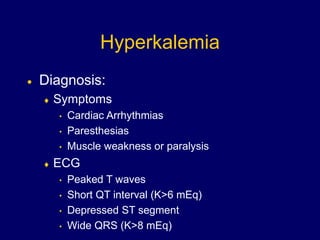
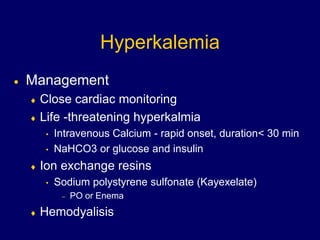
This document discusses fluid and electrolyte regulation and abnormalities in pediatrics. It covers the composition of body water compartments, daily fluid requirements, types of dehydration and their management, as well as electrolyte abnormalities including hyponatremia, hypernatremia, hypokalemia, and hyperkalemia. Signs and symptoms and treatment approaches are provided for each electrolyte imbalance.