This document discusses various techniques for assessing the physiological significance of coronary artery lesions seen on angiography. It describes:
1. Borderline or intermediate lesions that appear between 40-70% blocked on angiography but their physiological significance is unclear.
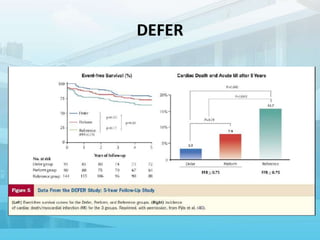
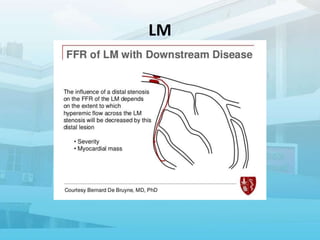
2. Various pressure-based indices that can be measured invasively using a wire, such as FFR, iFR, and others, to determine if a lesion is hemodynamically significant.
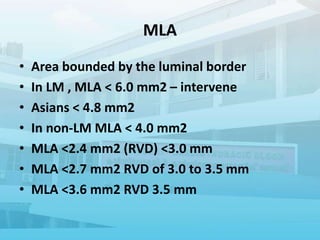
3. Additional modalities like IVUS and OCT that provide anatomical data to complement the functional assessment of lesions.