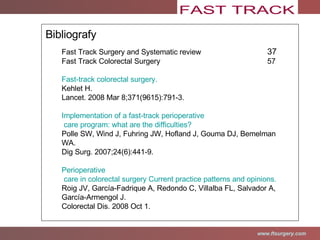
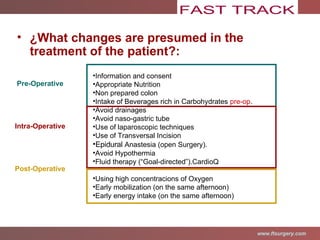
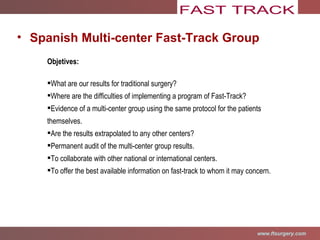
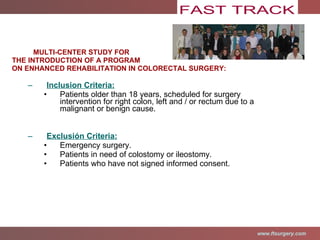
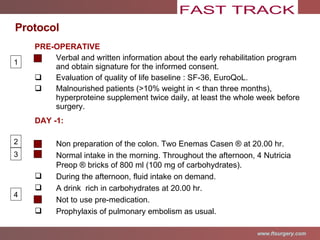
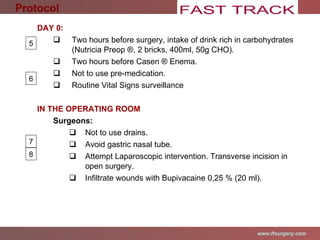
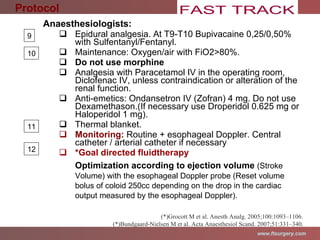
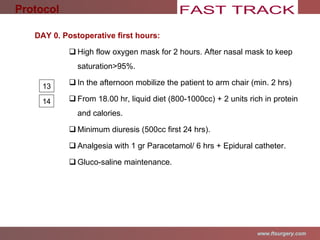
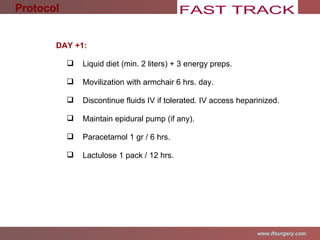
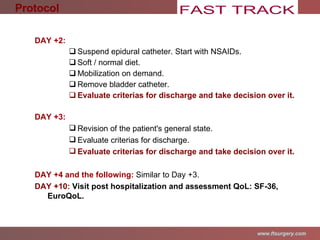
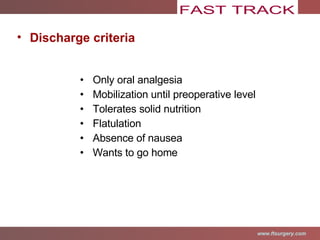
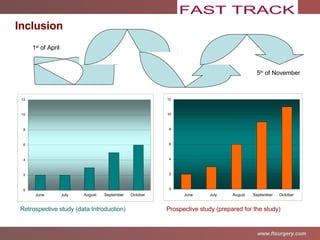
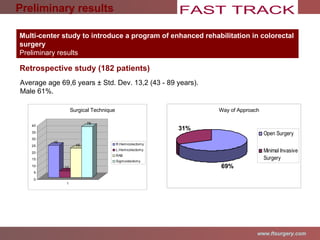
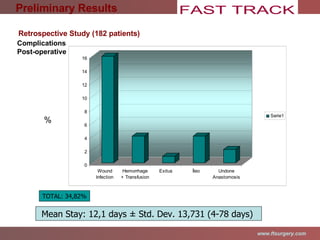
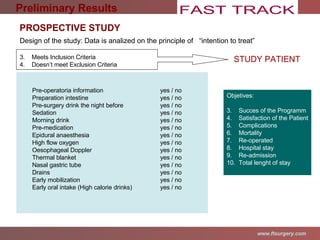
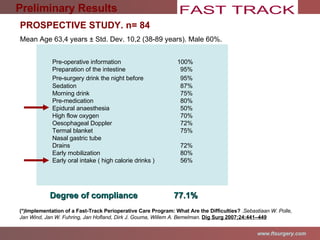
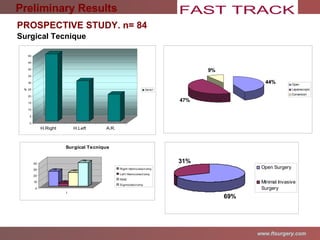
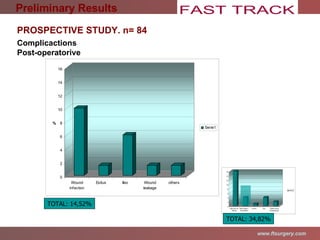
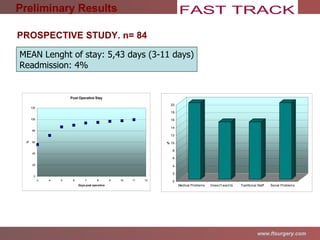
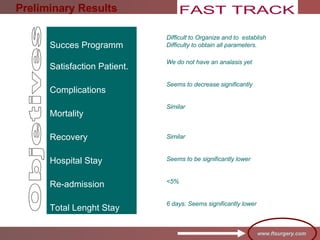
The document describes a multi-center study protocol and preliminary results for introducing an enhanced recovery program in colorectal surgery. The protocol aims to optimize pre-operative, intra-operative, and post-operative patient care and treatment to reduce morbidity, accelerate recovery, shorten hospital stays, and reduce costs. Preliminary retrospective results from one hospital show average length of stay was 12.1 days with 34.8% of patients experiencing complications. A prospective multi-center study will evaluate outcomes including success of the program, patient satisfaction, complications, mortality, re-operations, and readmissions.