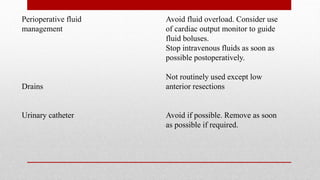
The document discusses Enhanced Recovery After Surgery (ERAS) protocols. It describes how ERAS aims to reduce surgical stress on patients through multimodal perioperative care, facilitating early recovery. This includes optimizations in pre-, intra-, and postoperative care such as shortened fasting times, carbohydrate loading, minimized fluid administration, and early mobilization. The document provides examples of procedures that can be done as day surgeries and details the key elements of ERAS protocols.