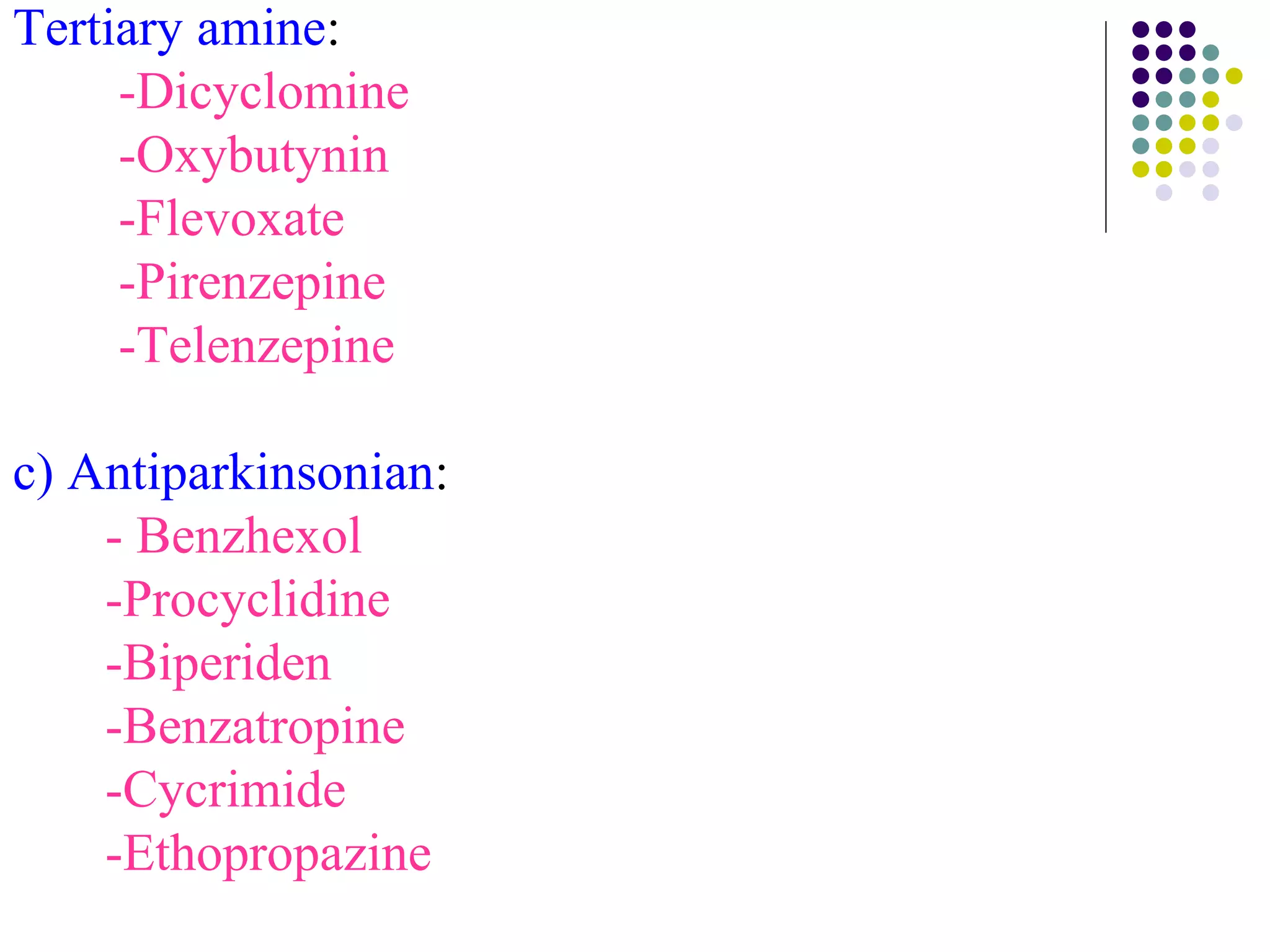
This document discusses anticholinergic drugs, including their classification, mechanisms of action, examples, and uses. It focuses on atropine as the prototype anticholinergic. Atropine is a competitive muscarinic receptor antagonist derived from deadly nightshade. It has various pharmacological effects throughout the body mediated by blocking acetylcholine actions at muscarinic receptors in the CNS, cardiovascular system, gastrointestinal tract, respiratory system, and other areas. Adverse effects and clinical uses of atropine and other anticholinergic drugs are also summarized.