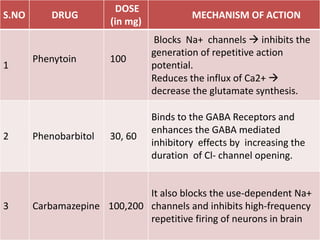
Epilepsy is a neurological disorder characterized by recurrent seizures caused by excessive neuronal activity in the brain. A seizure occurs when nerve cell activity in the brain is disturbed, causing changes in movement, behavior, sensation (including "auras"), or consciousness. Epilepsy is defined as having two or more unprovoked seizures. Seizures have many potential causes including genetics, brain injury, and unknown factors. Treatment involves medications called anti-epileptic drugs which help control seizures by various mechanisms such as enhancing GABA inhibition or blocking sodium channels. Diagnosis involves a detailed history and examination, and may include tests like EEG, MRI, and genetic testing.