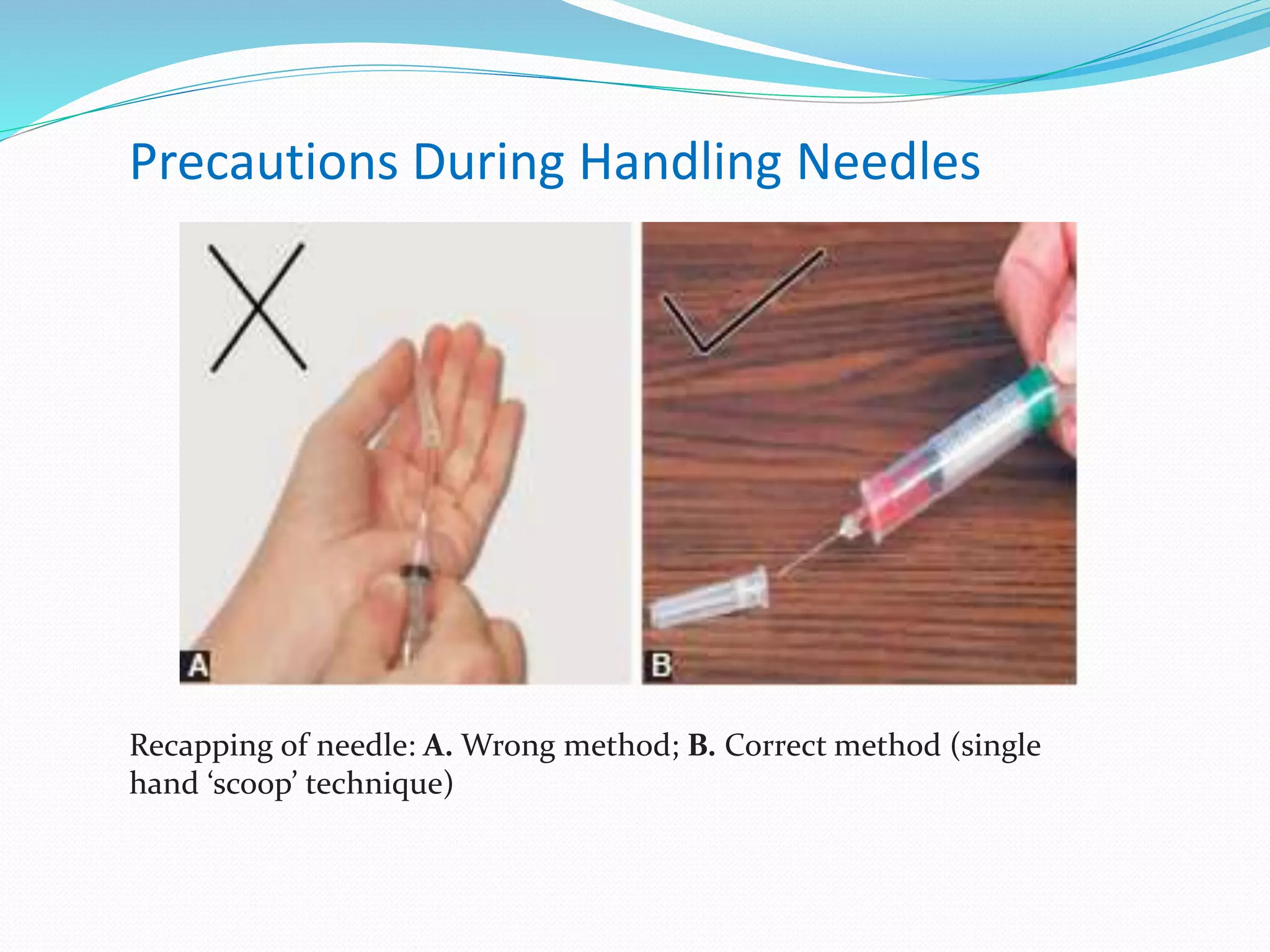
A needle stick injury is a penetrating wound from a contaminated sharp object that may expose a healthcare worker to infectious diseases. Nurses experience 43% of injuries, usually occurring in patient rooms during use of devices like disposable syringes. Proper handling and disposal of sharps can prevent injuries. If exposed, first aid and post-exposure prophylaxis based on injury type lowers risk of transmitting bloodborne viruses like HIV, HBV, and HCV. Eliminating unnecessary sharps use, training safe practices, and using safety devices can further reduce healthcare worker risk.