This document provides an overview of electrical stimulation including:
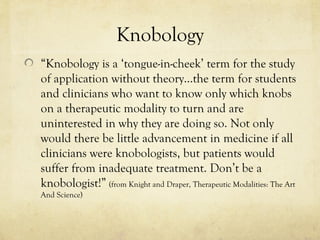
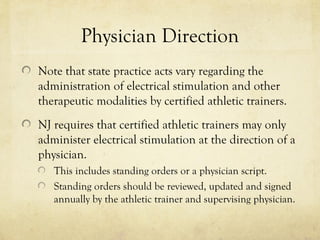
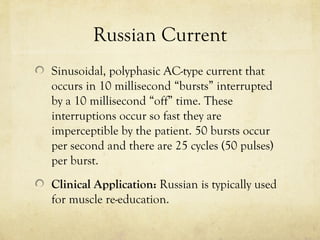
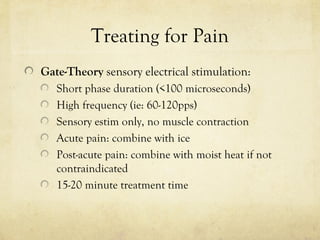
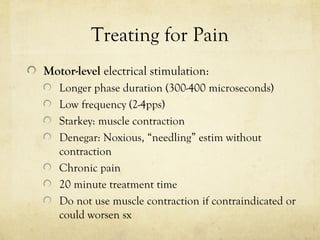
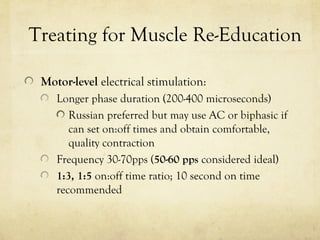
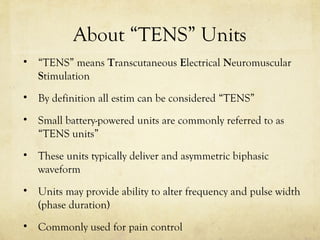
- Definitions of terms like knobology, different current types (AC, DC, pulsed), and reasons for using electrical stimulation like pain reduction and muscle re-education.
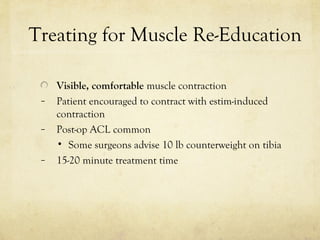
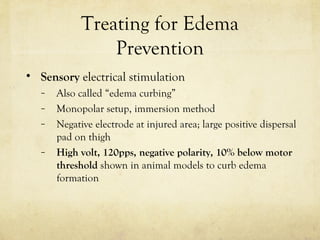
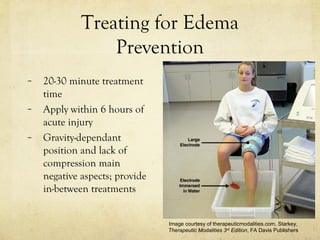
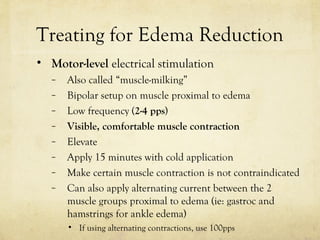
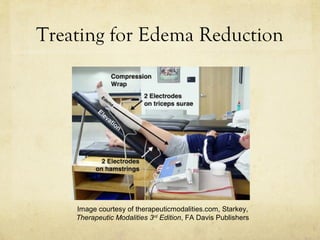
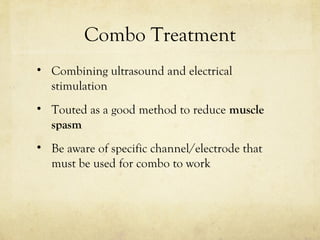
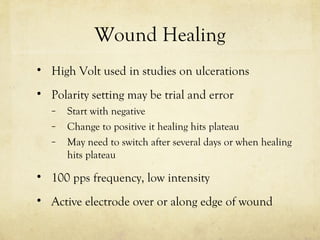
- Guidelines for treating pain, muscle re-education, edema prevention and reduction with electrical stimulation.
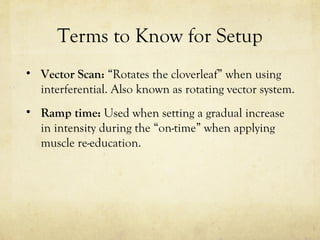
- Details on setup terms like amplitude, frequency, and duty cycle.
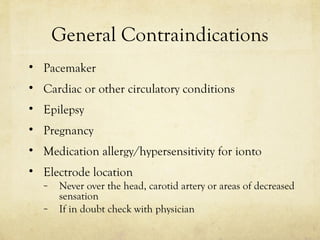
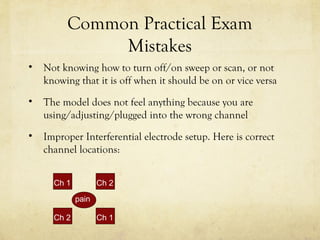
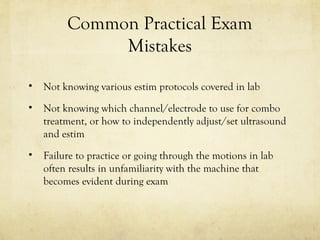
- Contraindications and common mistakes to avoid.
- References for further information.