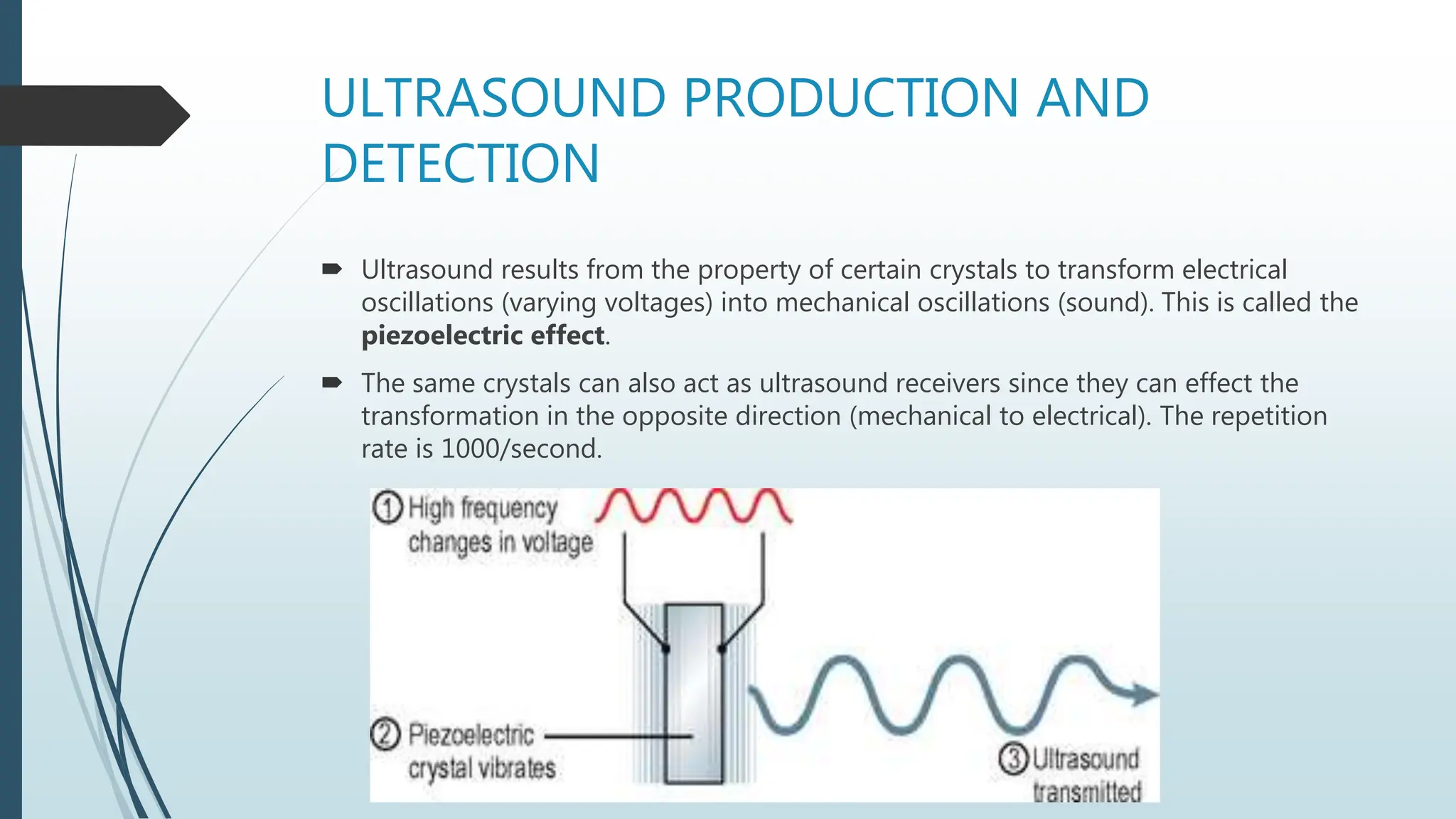
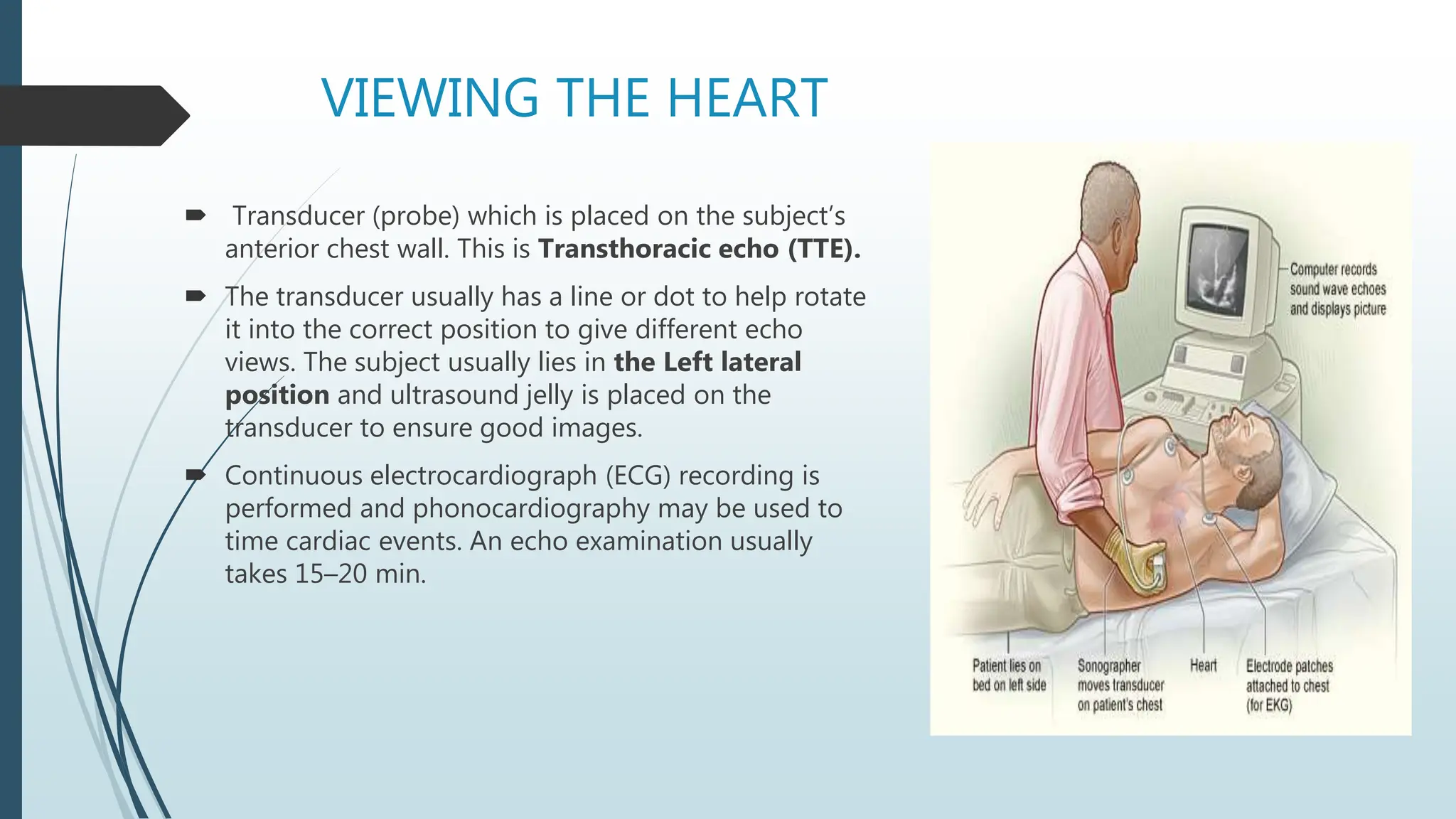
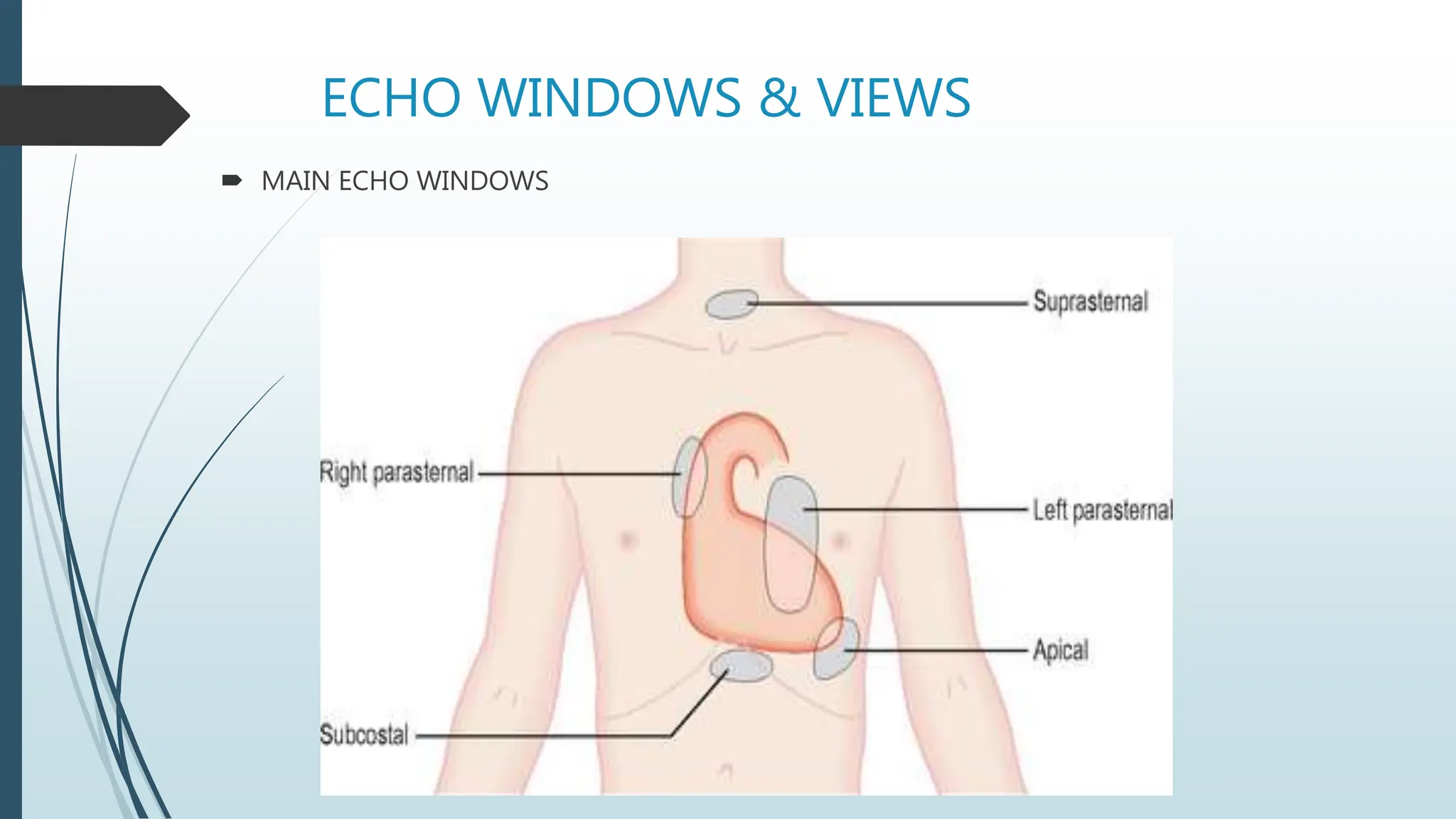
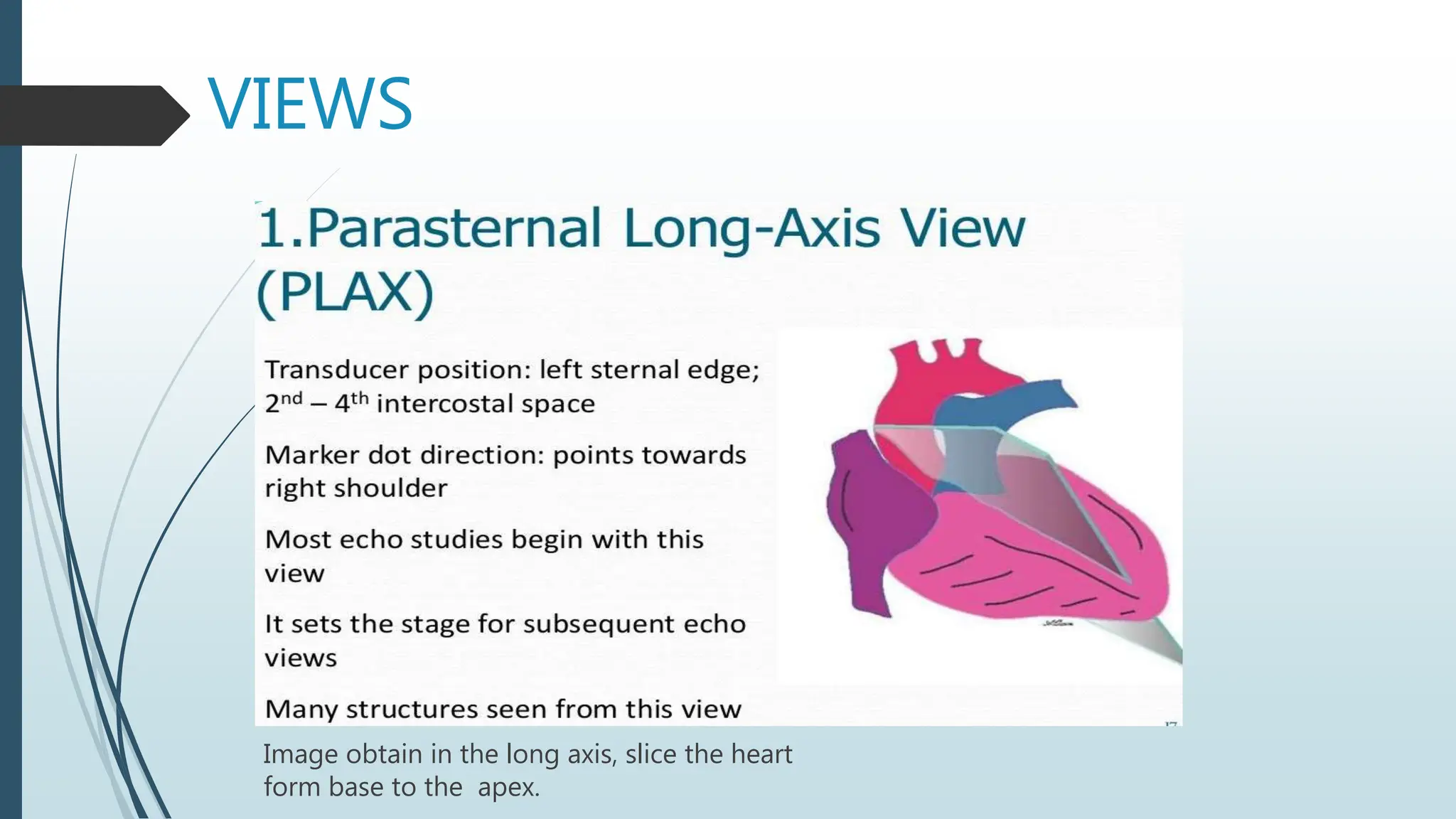
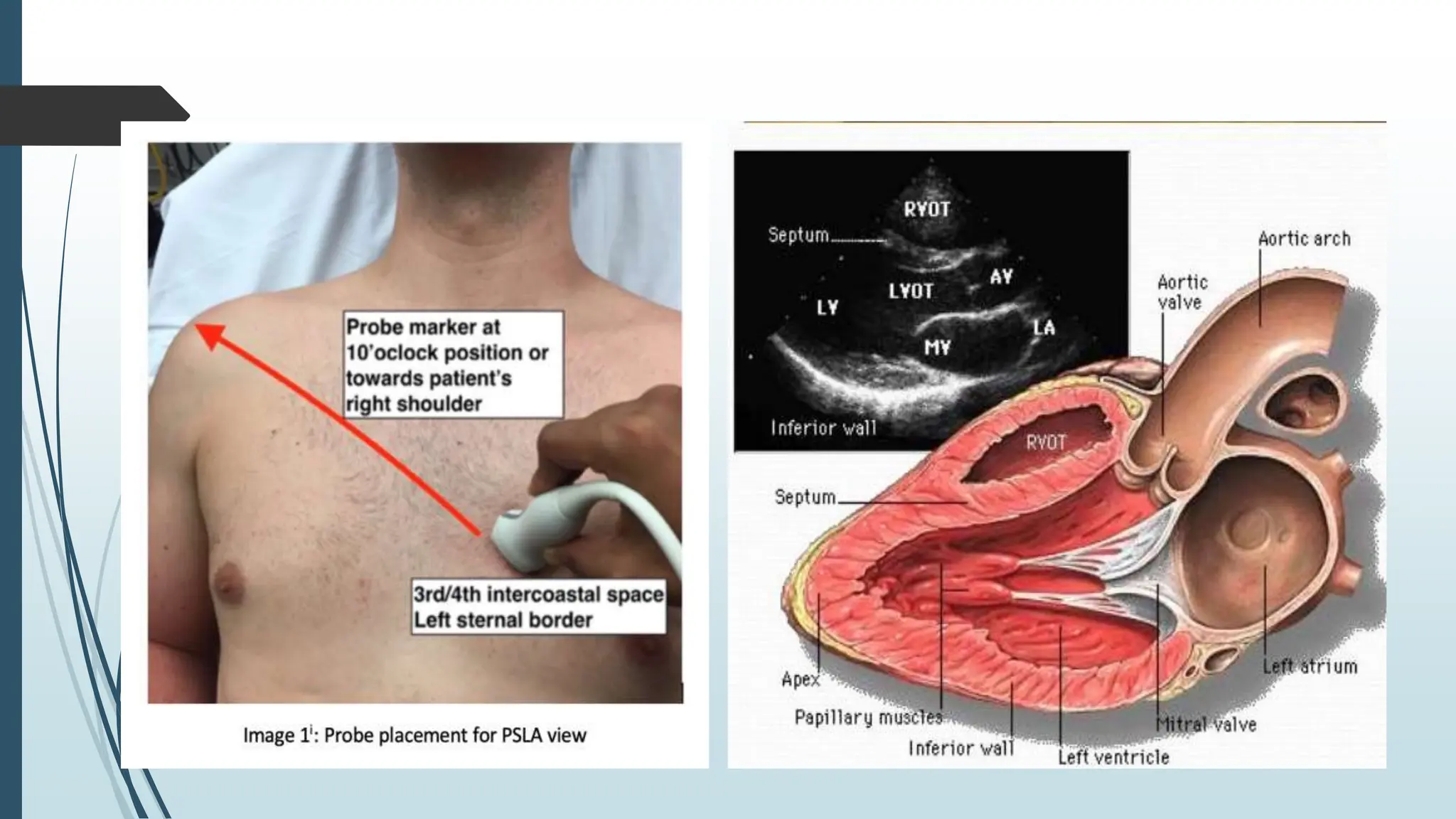
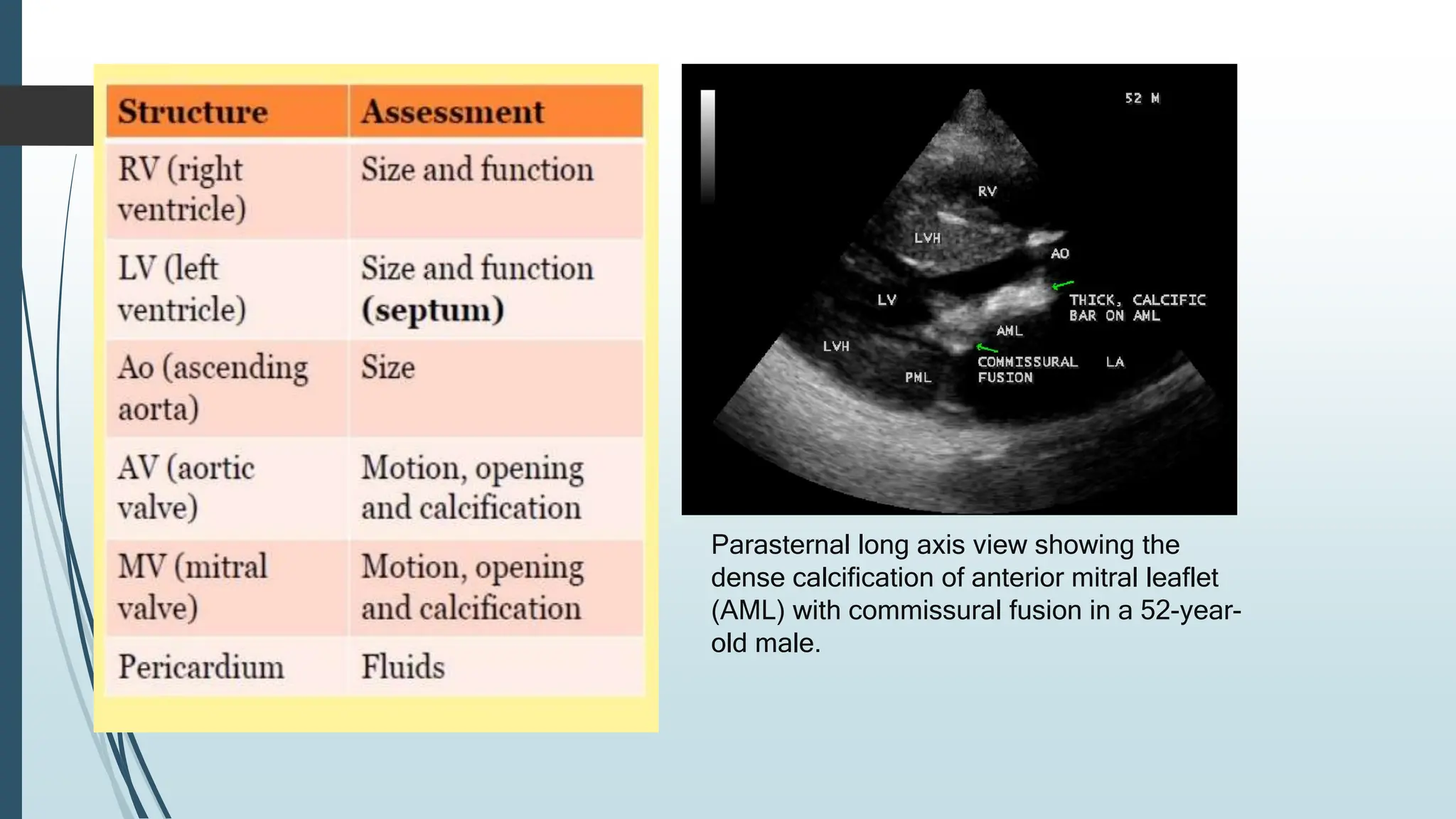
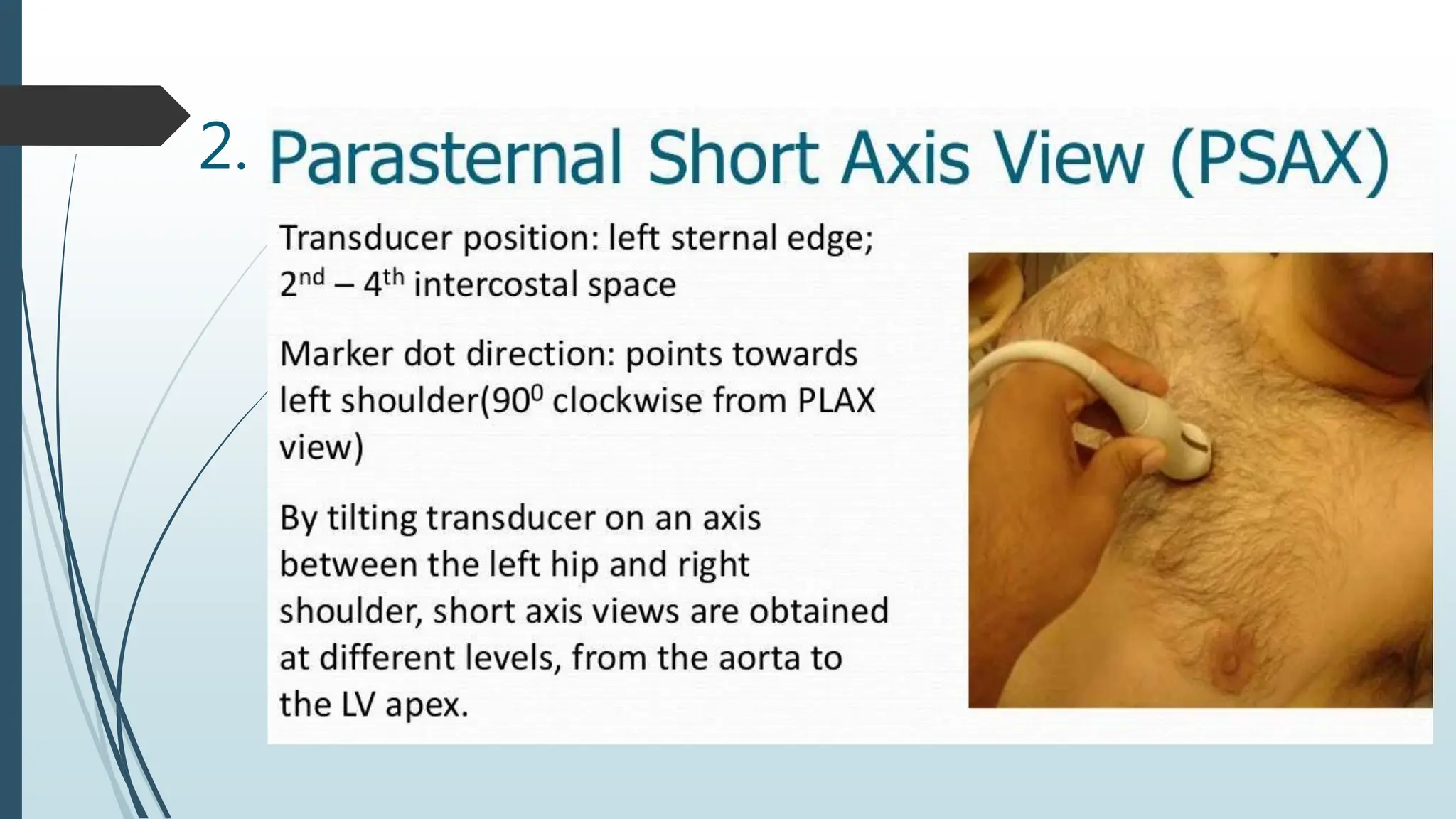
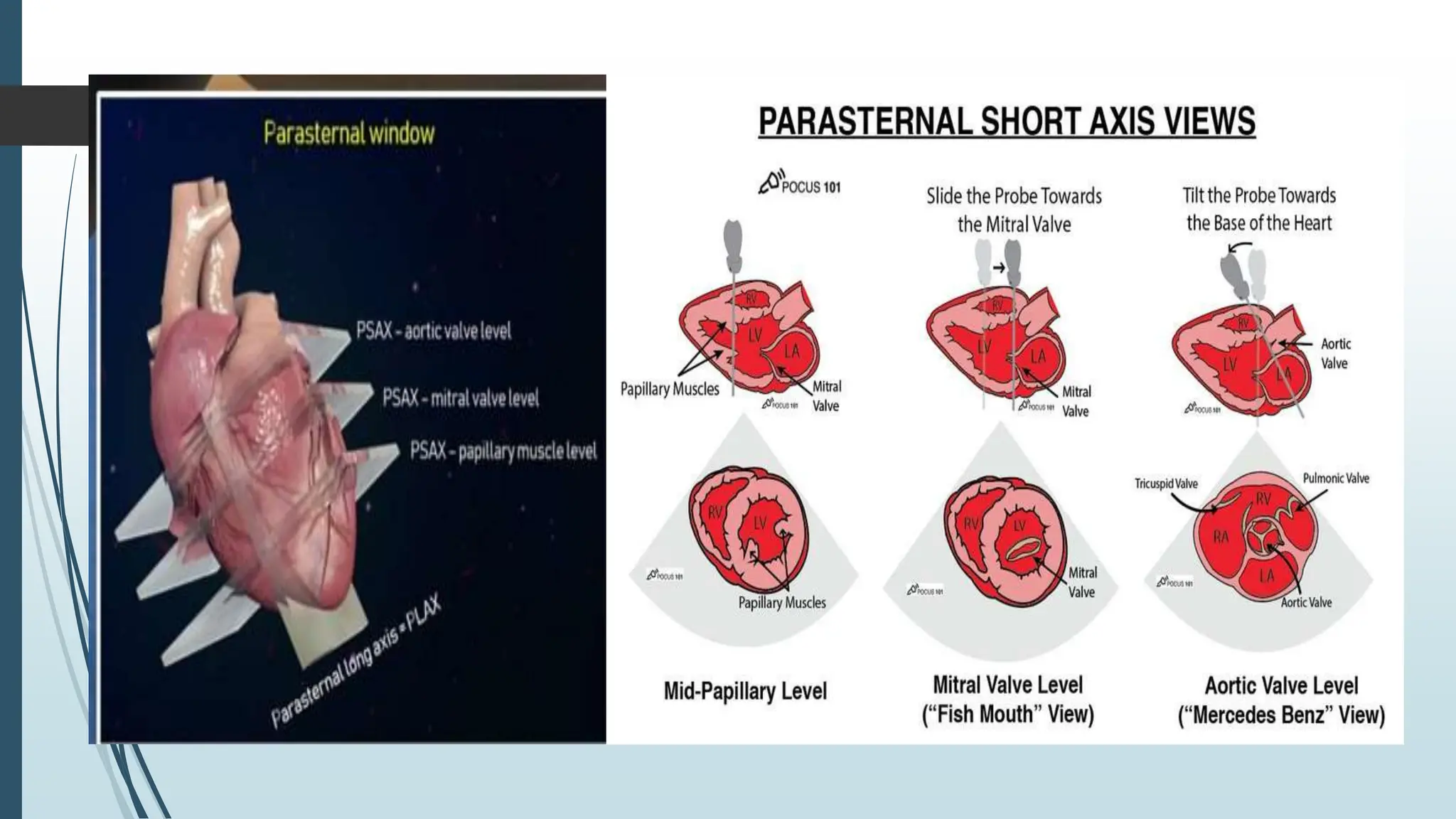
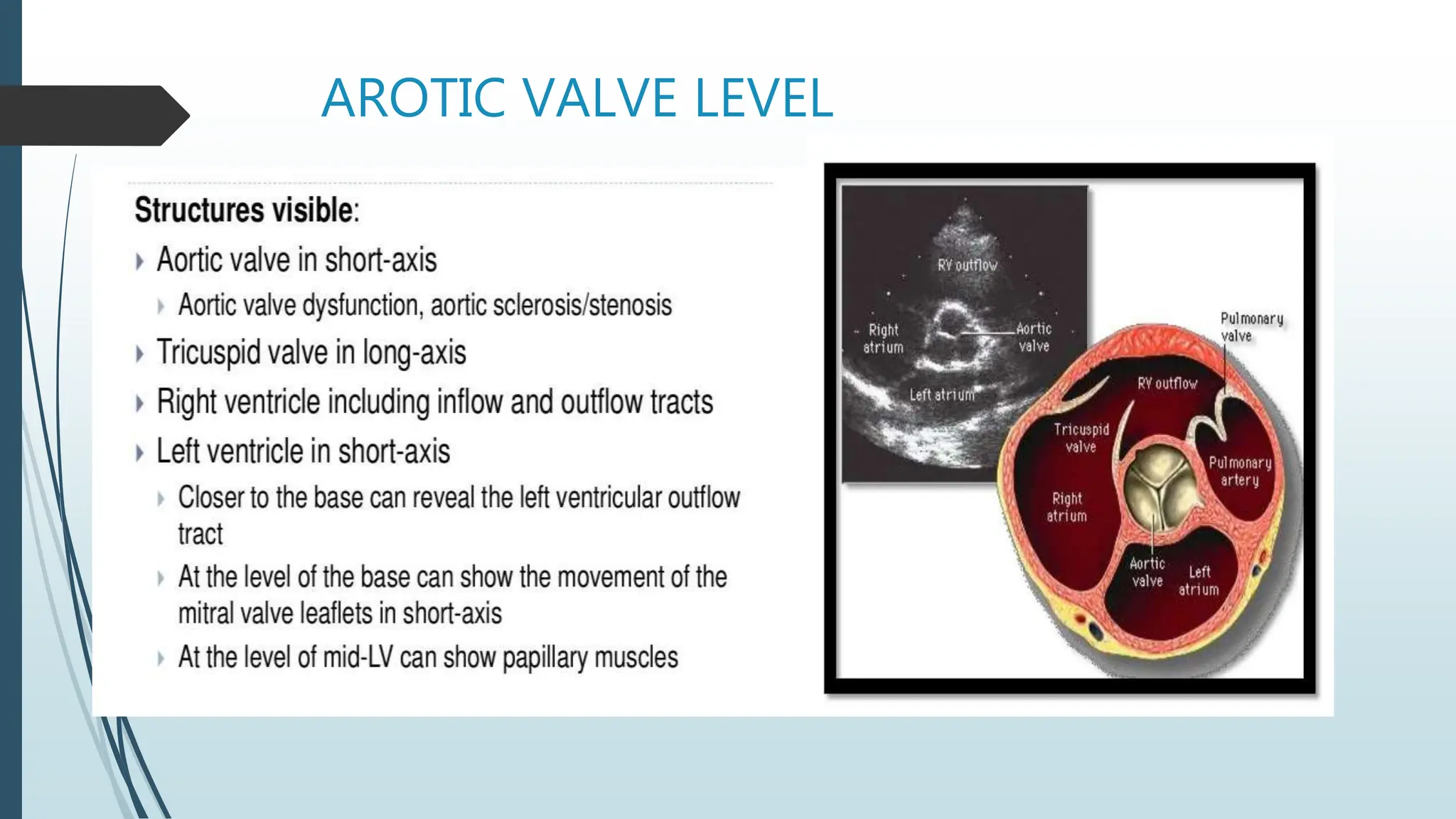
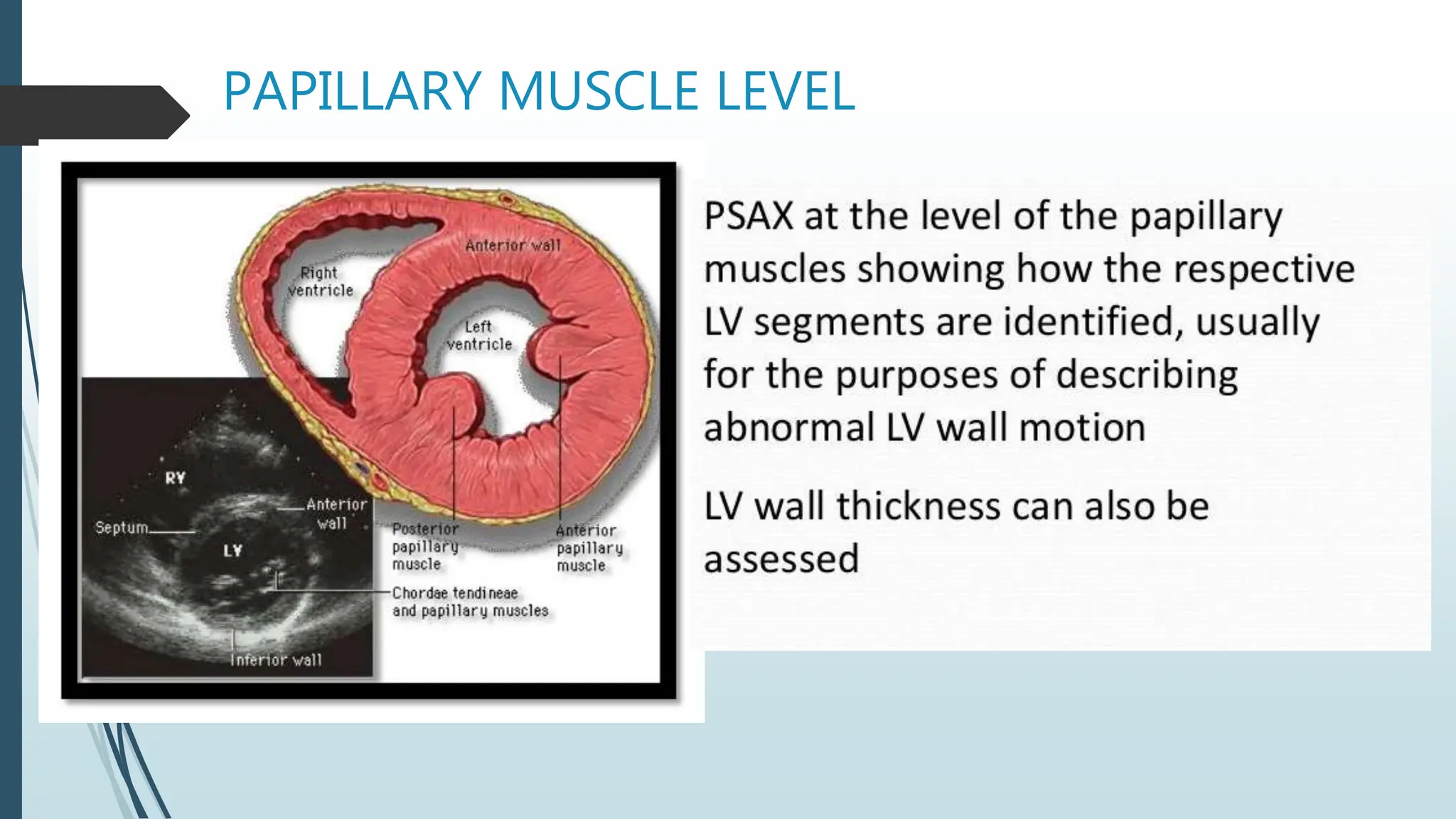
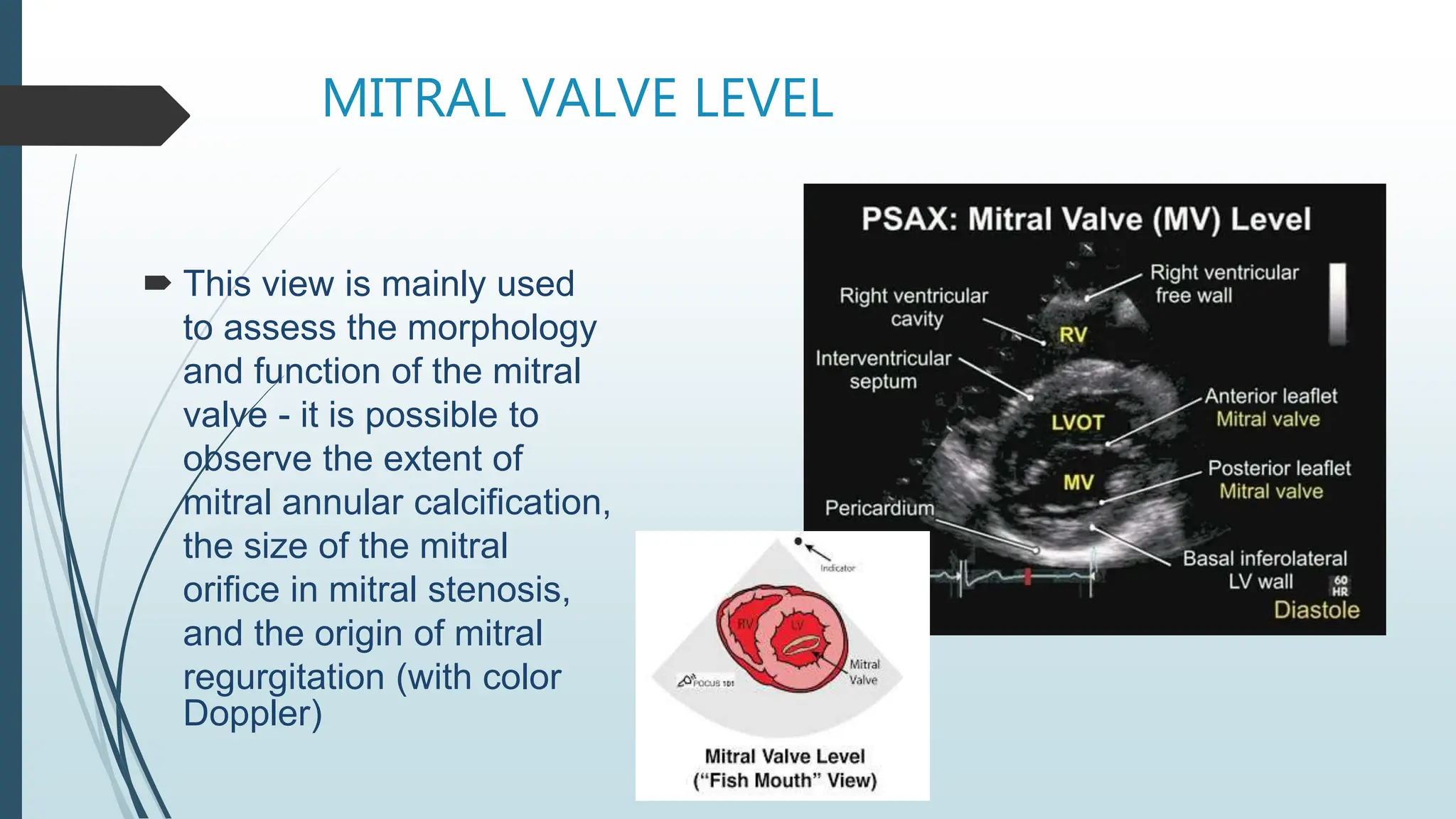
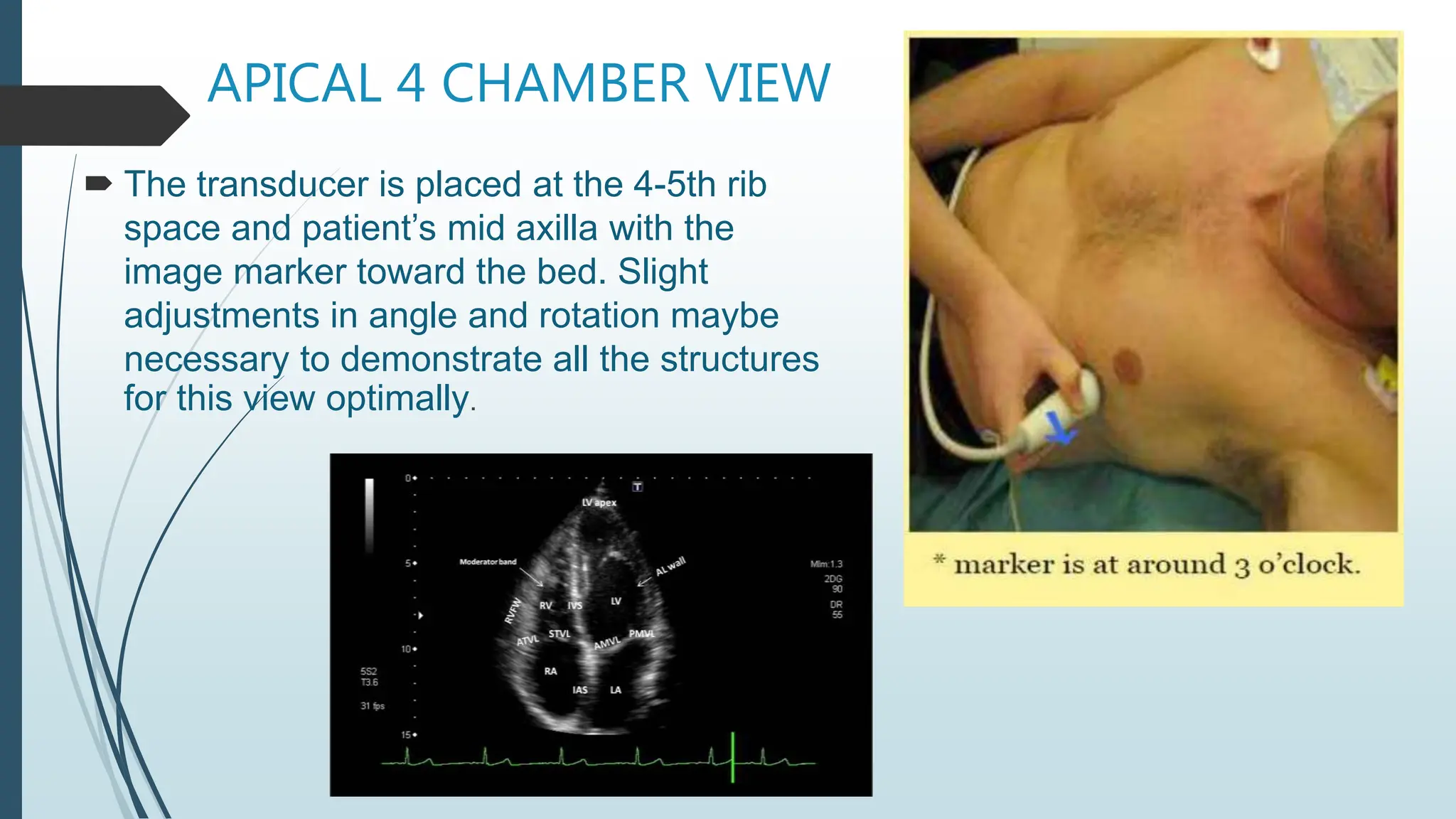
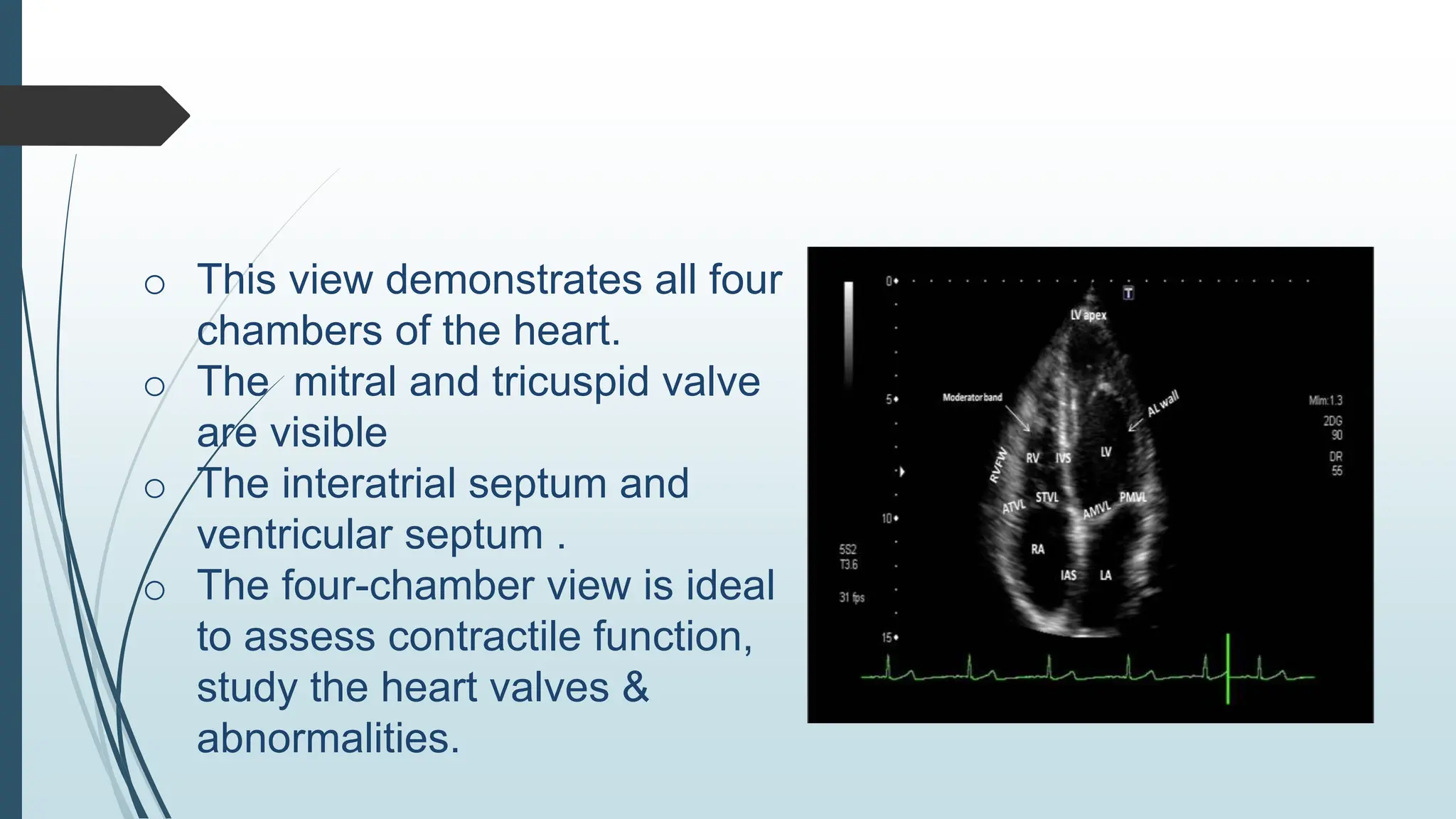
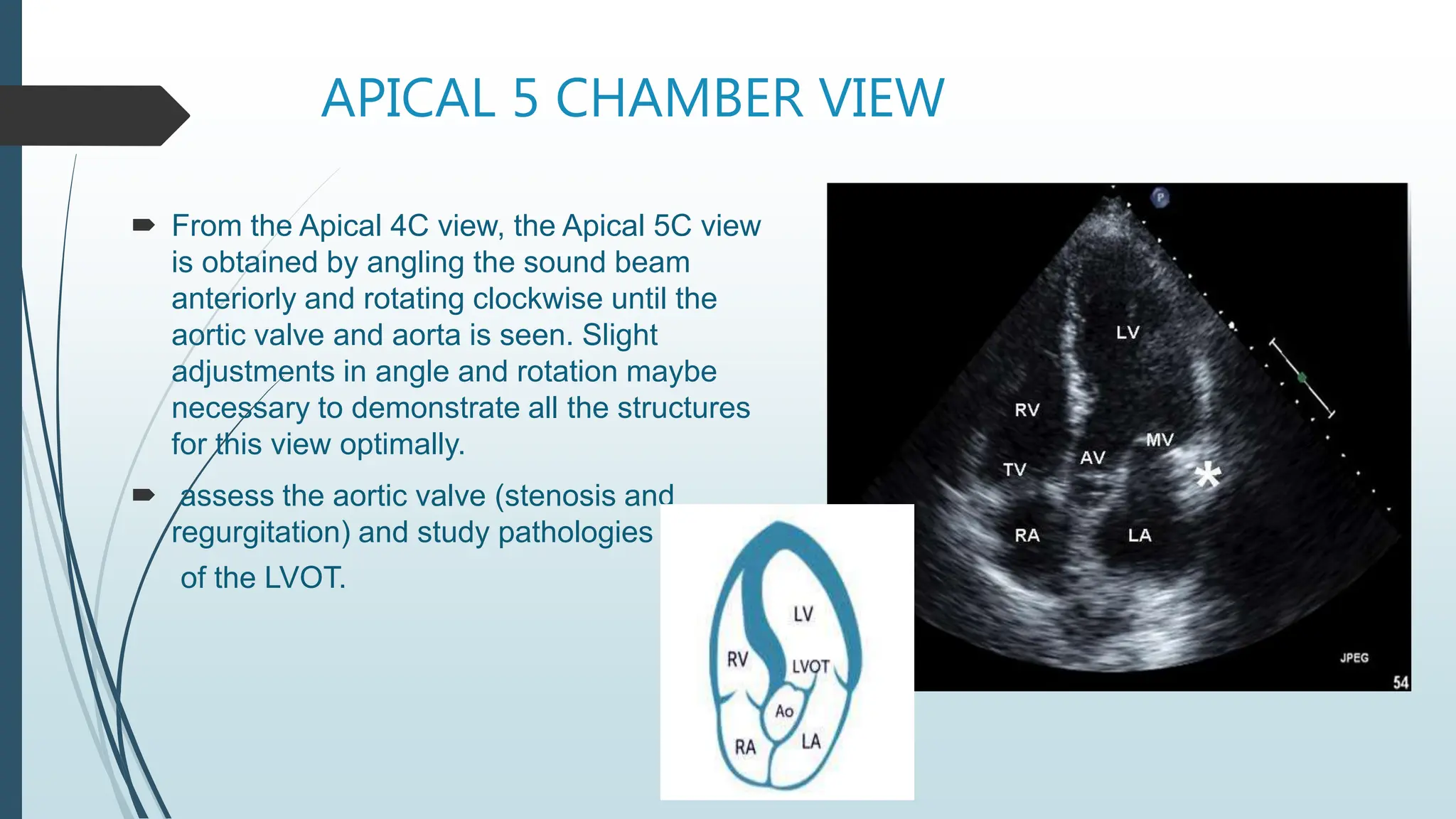
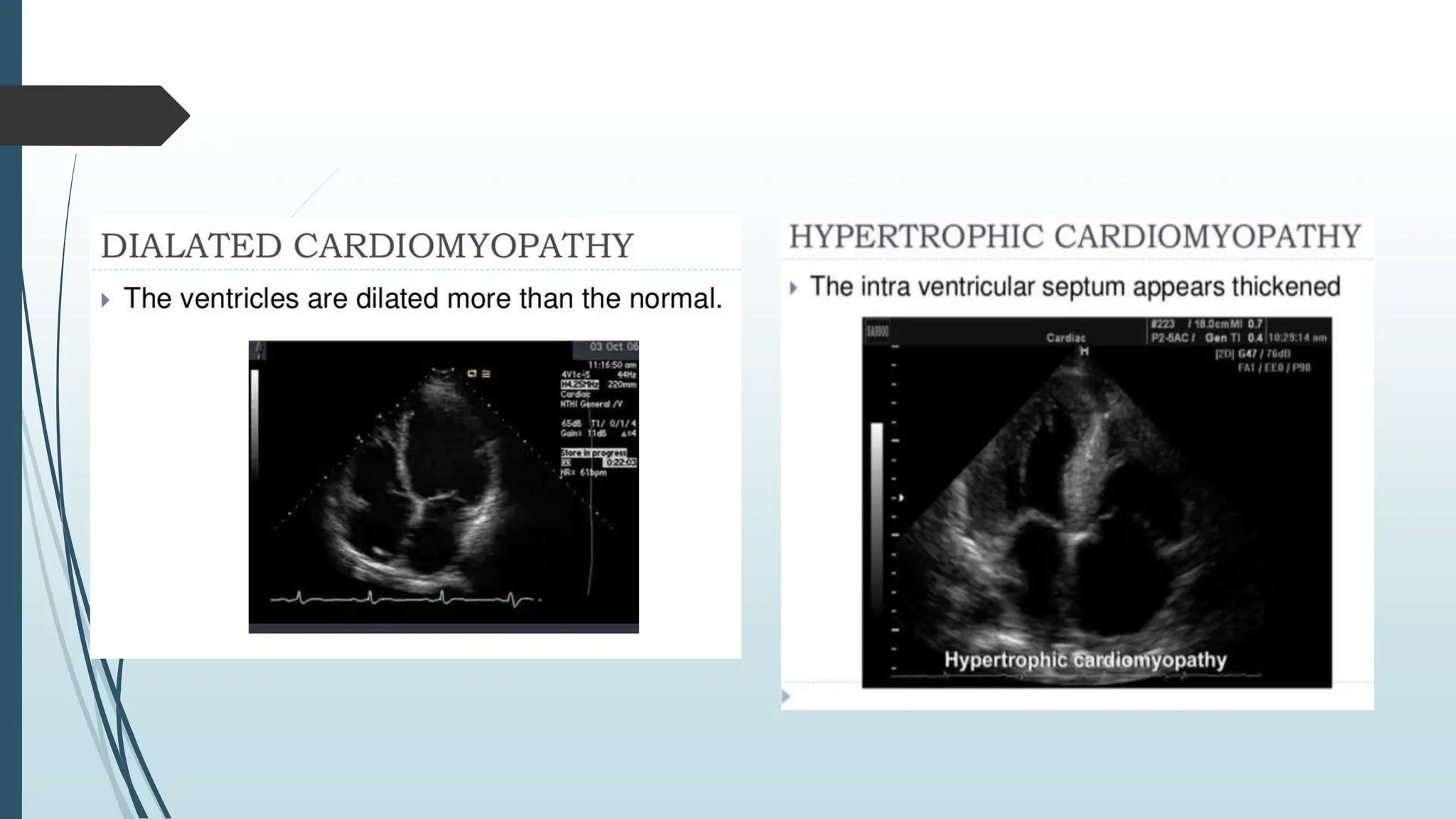
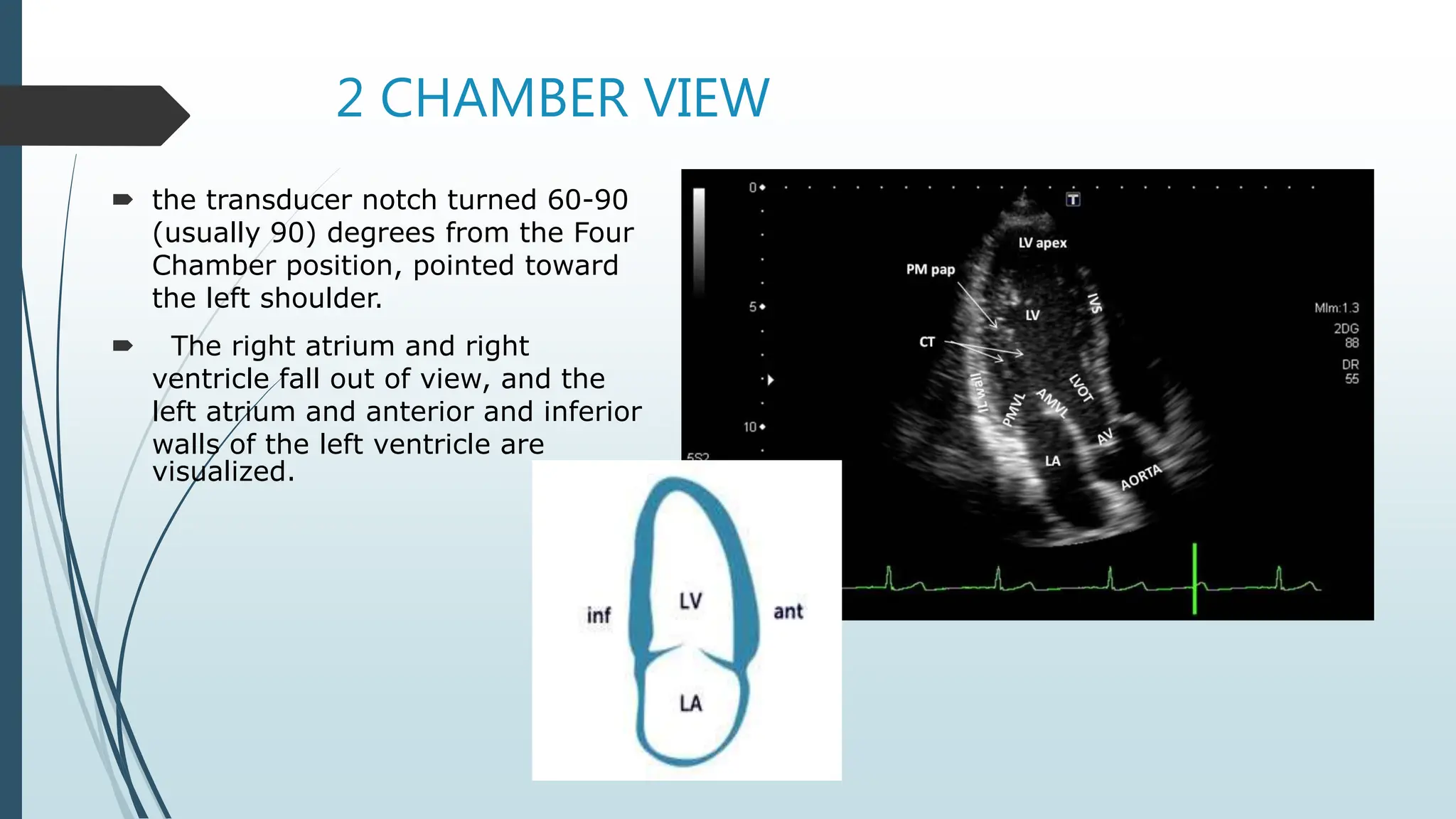
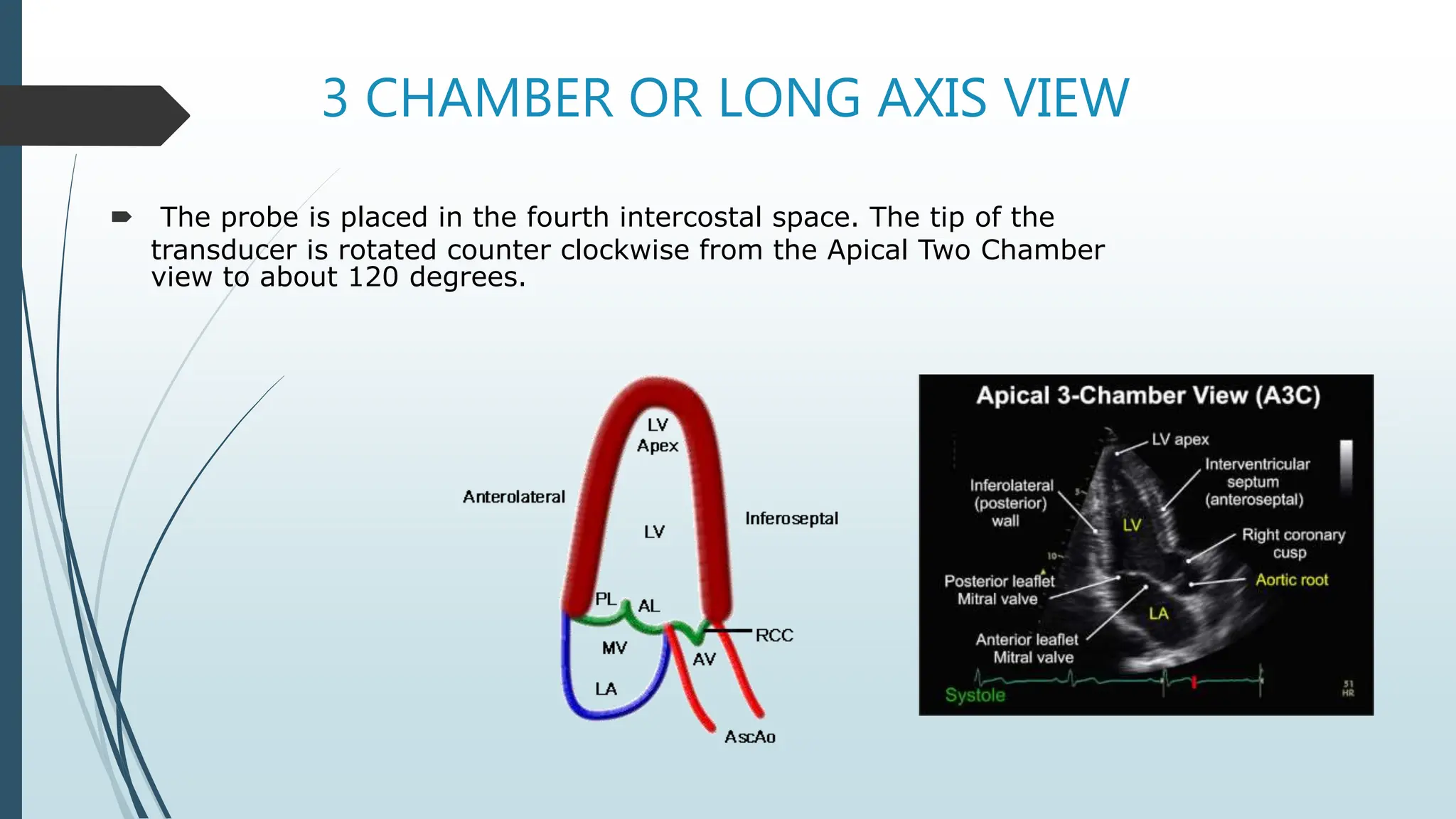
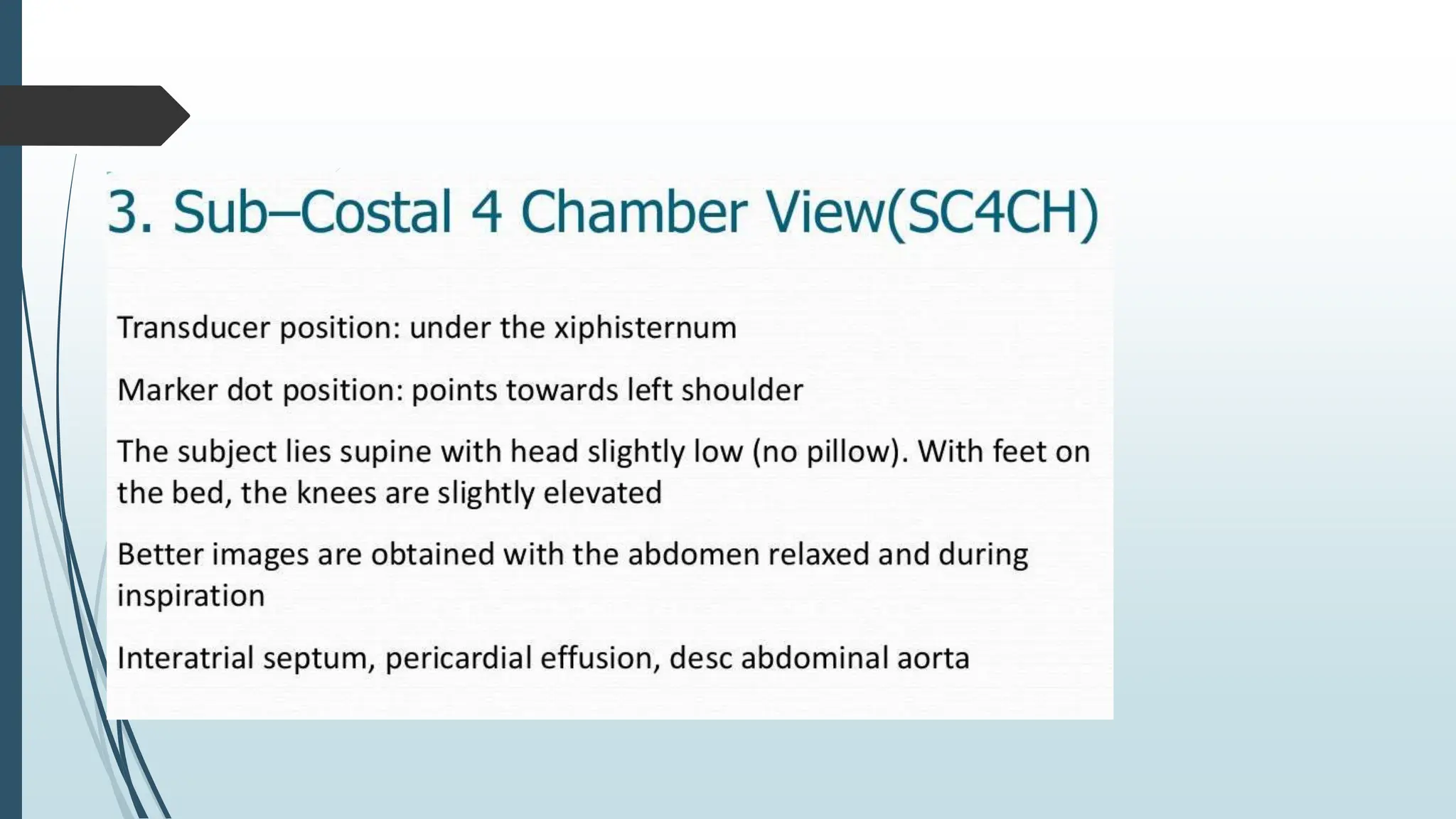
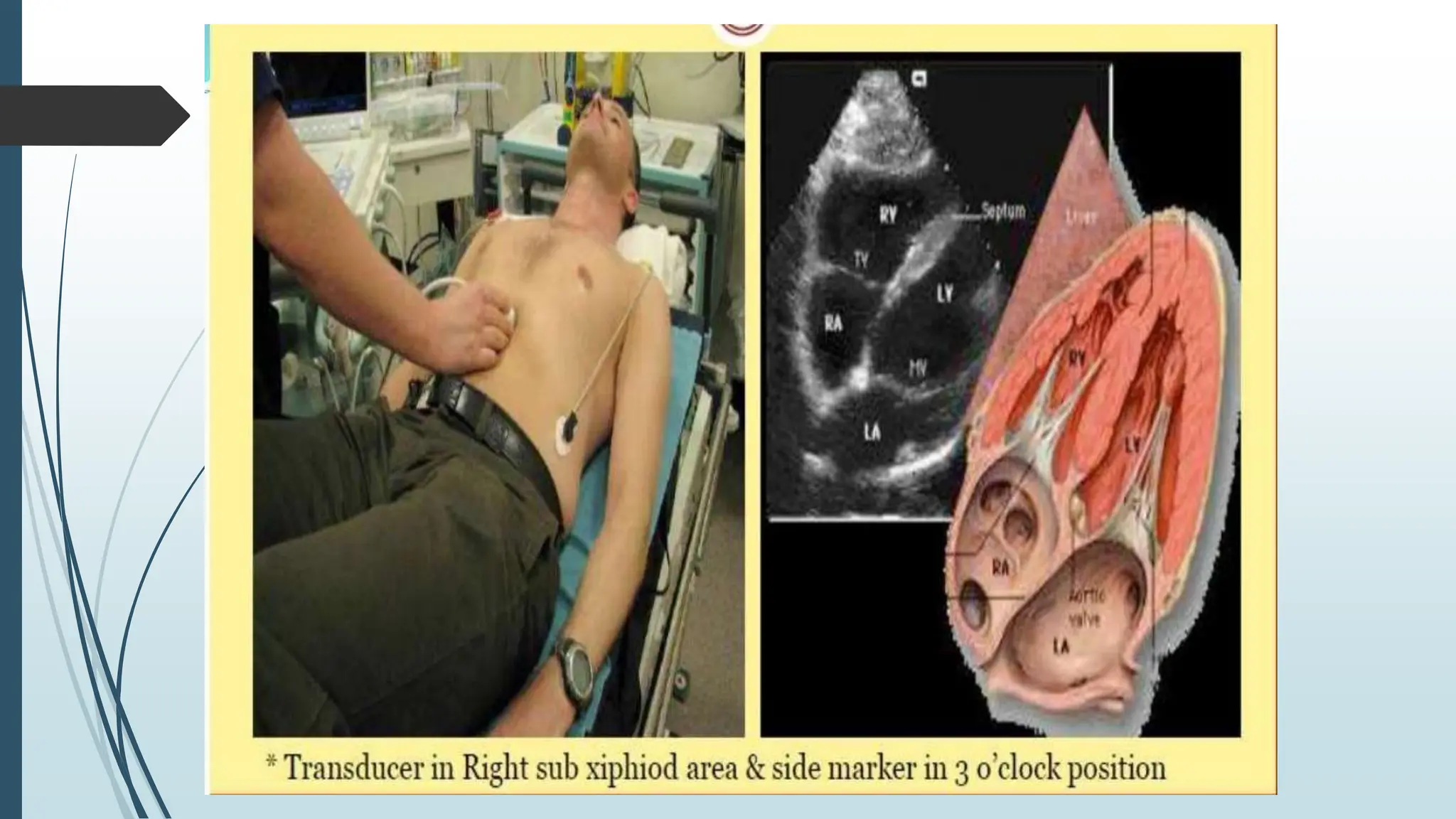
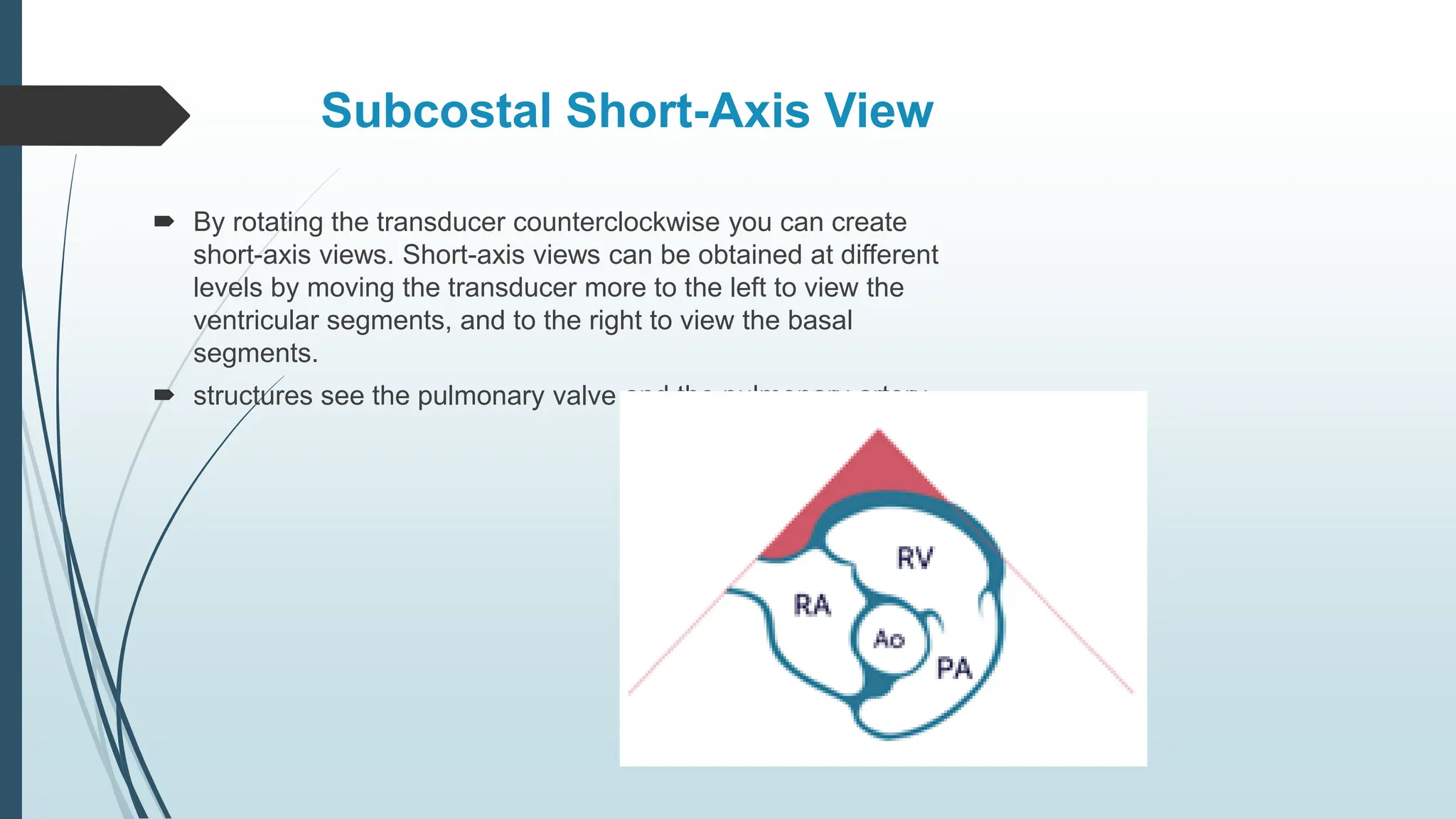
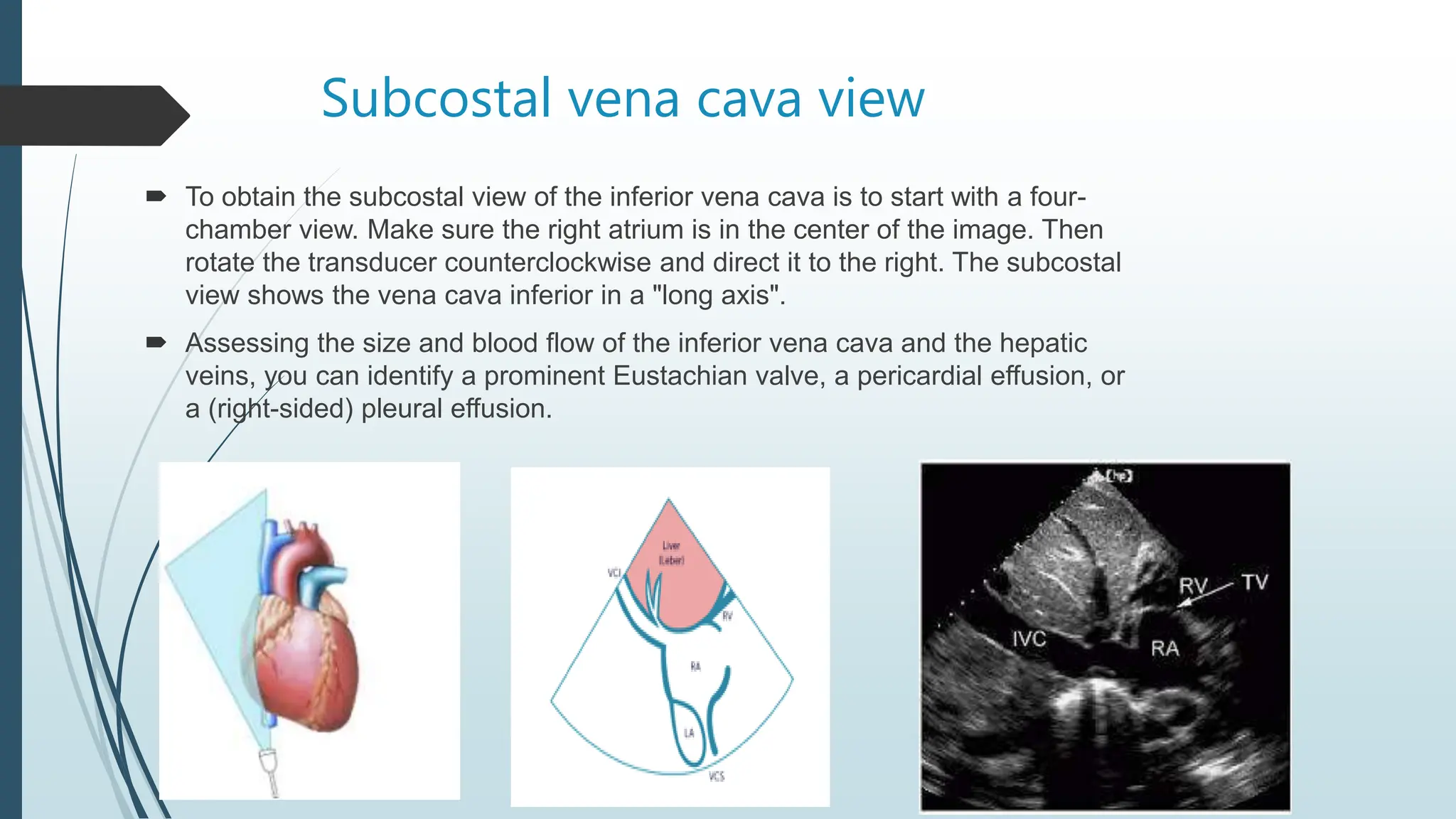
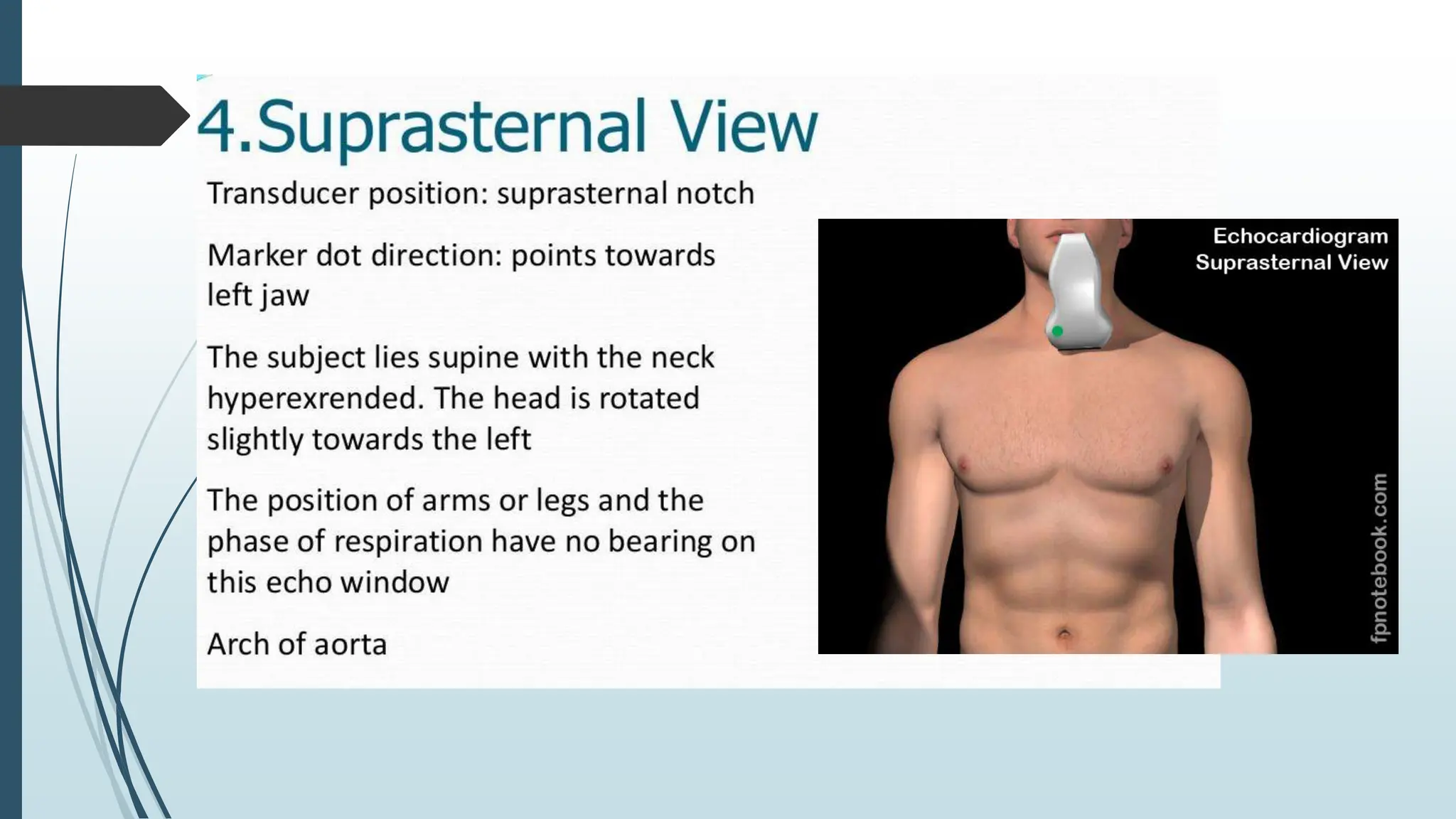
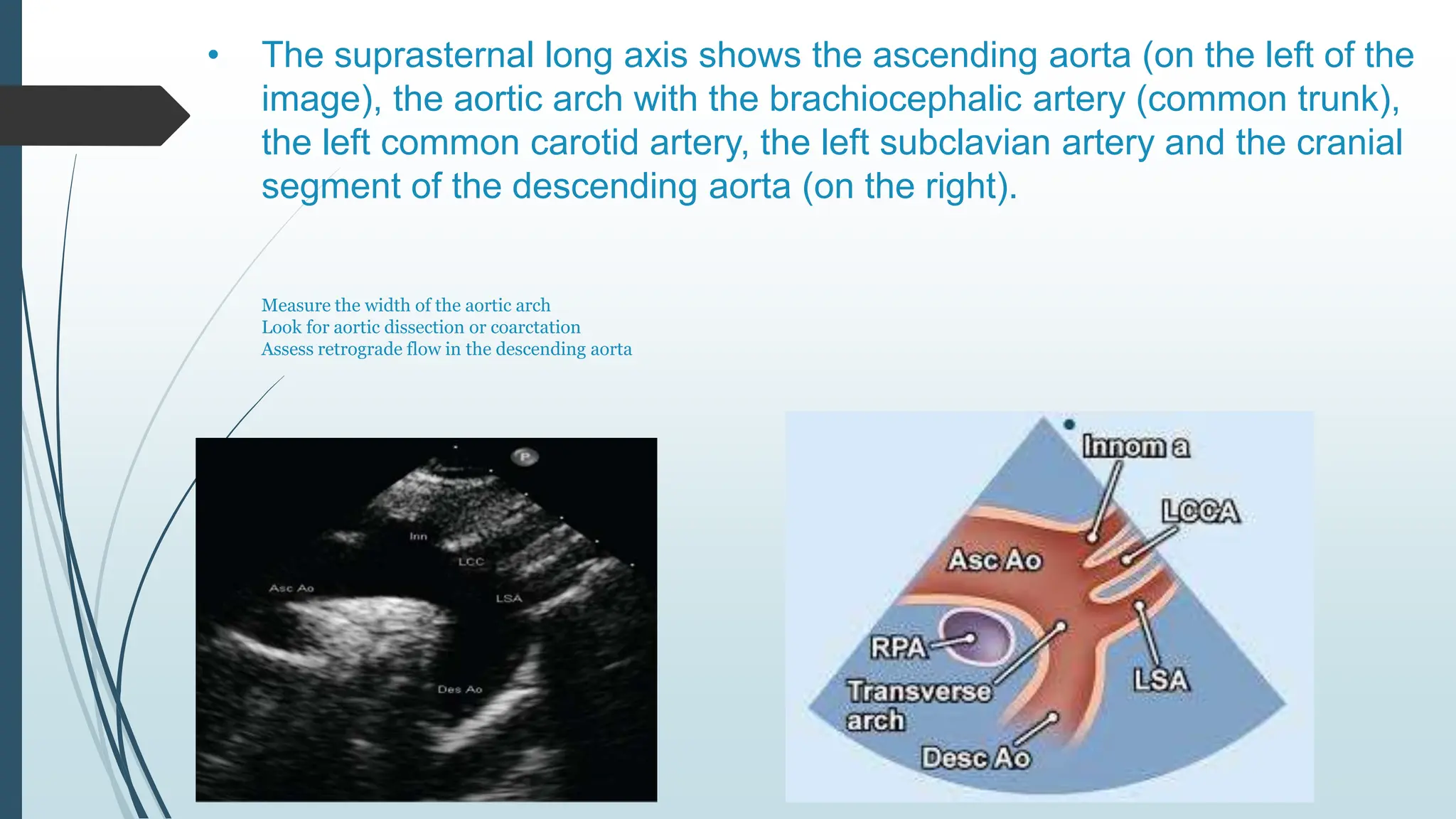
The document provides an overview of echocardiography, a medical imaging technique using ultrasound to assess heart conditions, including heart chambers, pumping capacity, and valve function. It details the principles behind echocardiography, the equipment used (transducer), and various echocardiographic views such as parasternal long axis, apical four-chamber, and subcostal views, each with specific applications in diagnosing heart conditions. The document emphasizes the process of capturing and interpreting heart images to aid in clinical assessments.