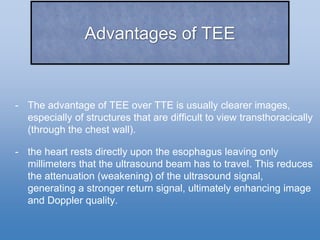
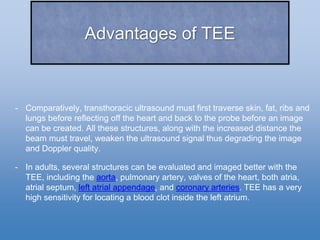
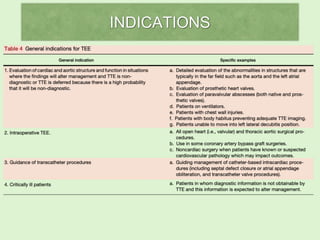
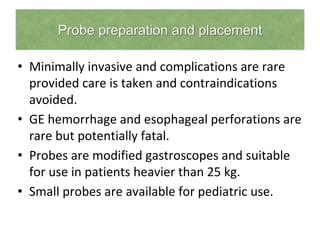
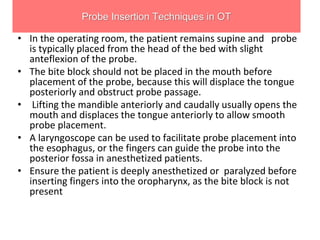
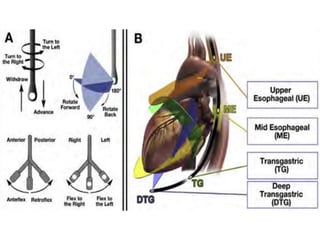
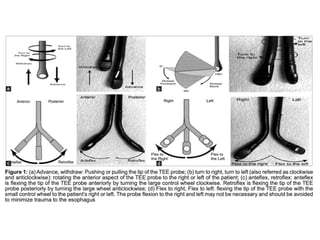
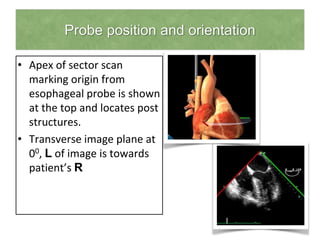
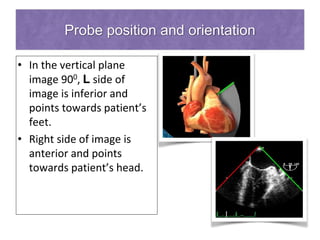
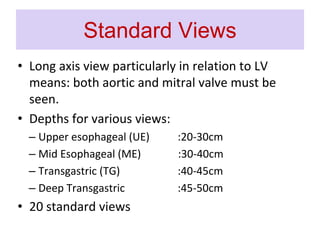
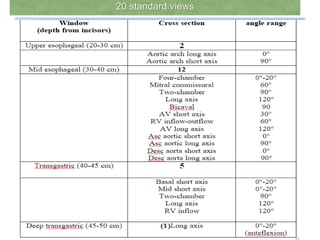
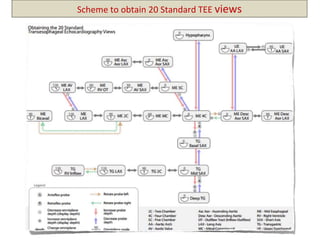
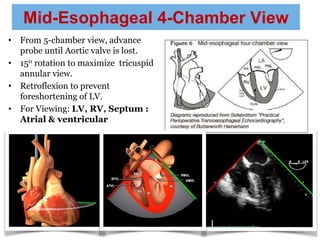
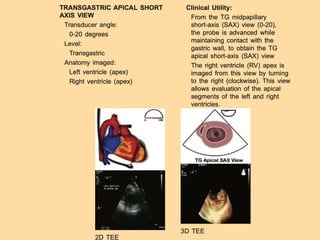
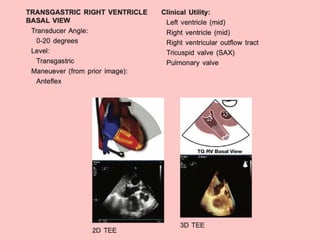
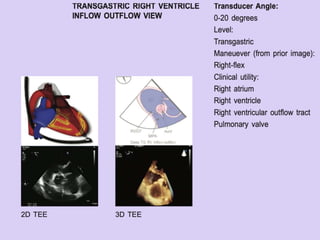
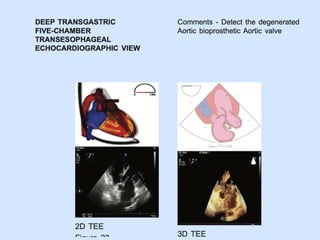
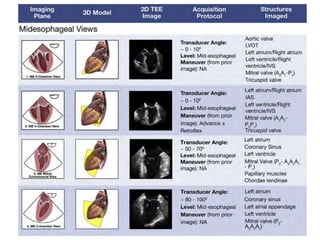
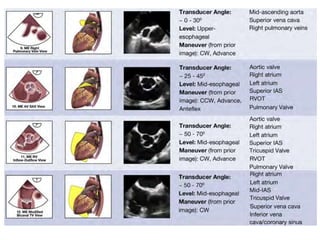
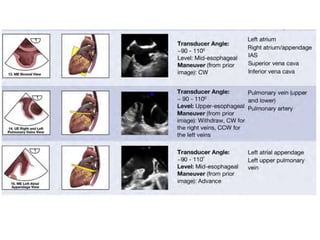
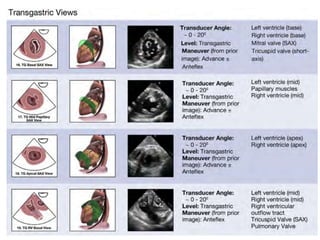
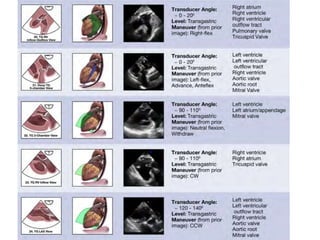
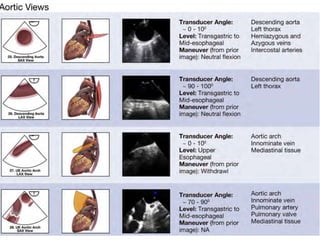
TEE provides clearer images of the heart compared to TTE due to the closer proximity of the esophagus to the heart. Some structures like the aorta, pulmonary artery and valves are better visualized with TEE. The standard TEE exam involves obtaining 20 predefined views of the heart from the mid-esophageal position and transgastric position. These views allow thorough examination of the valves, chambers, great vessels and other cardiac structures. Precautions must be taken when performing TEE to avoid complications like esophageal perforation.