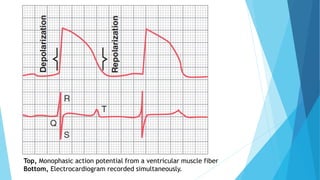
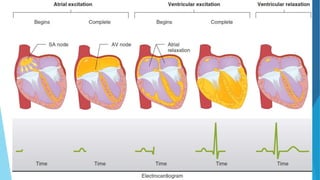
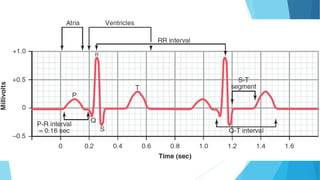
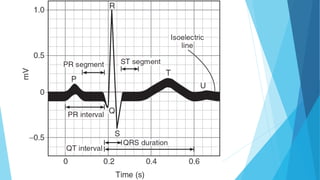
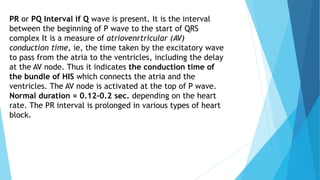
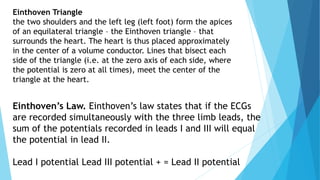
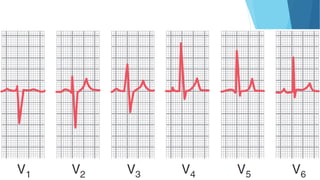
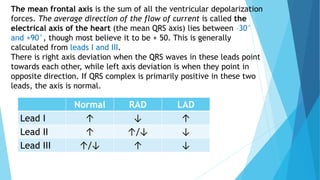
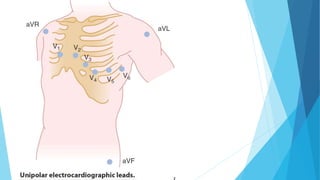
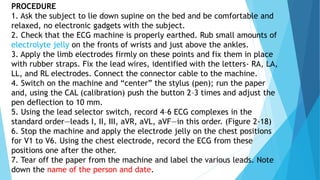
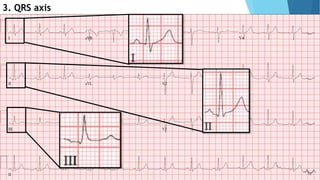
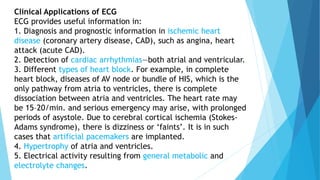
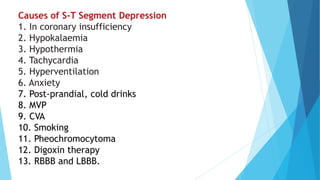
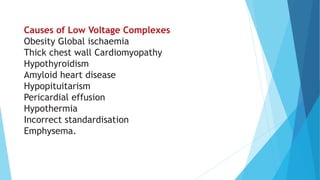
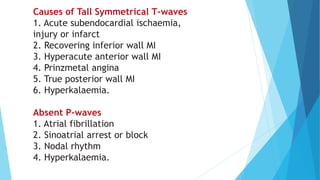
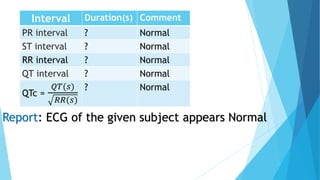
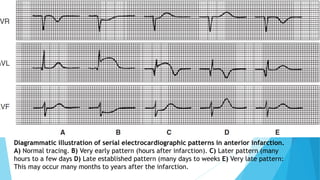
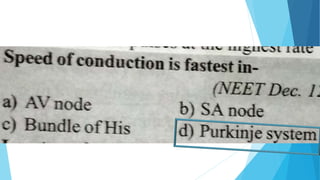
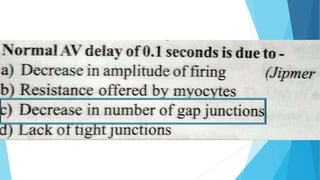
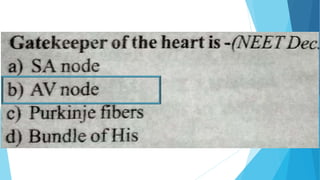
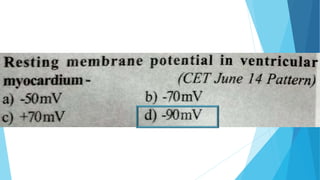
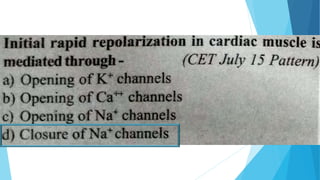
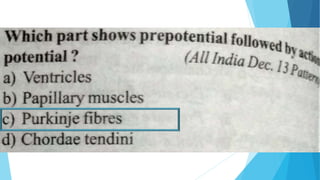
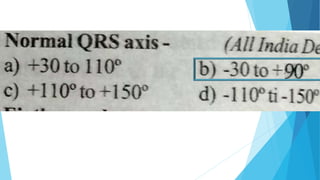
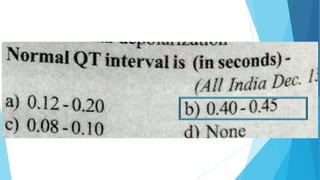
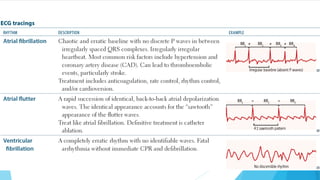
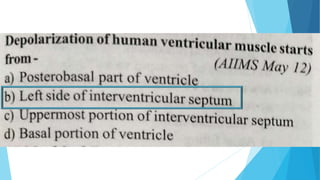
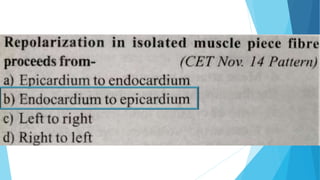
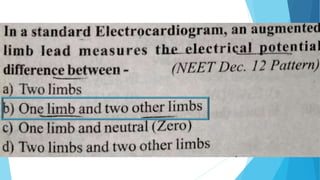
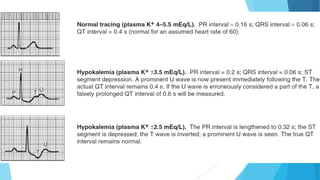
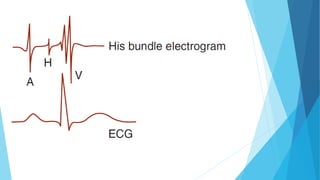
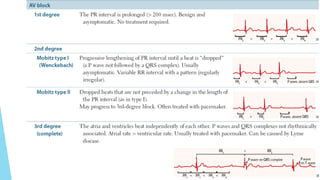
This document discusses the electrocardiogram (ECG) and its components. It begins by describing the myocardial action potential and its phases. It then discusses the pacemaker action potential and ECG waves including the P, QRS, T, and U waves. It explains ECG intervals such as the PR, QT, and ST segments. The document also covers ECG leads, normal values, procedures for recording an ECG, interpreting ECG findings, and clinical applications of the ECG.