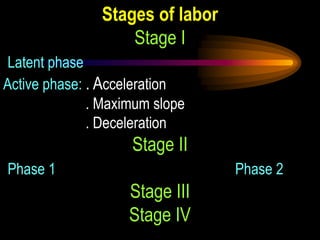
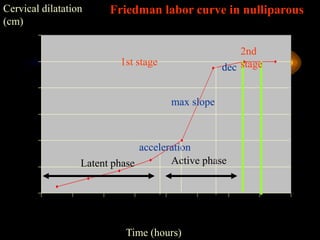
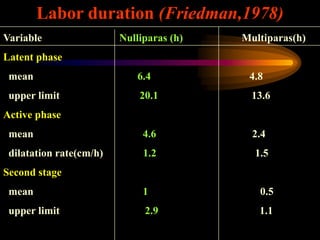
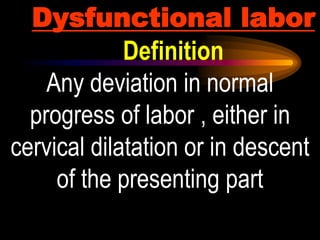
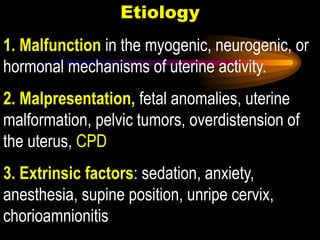
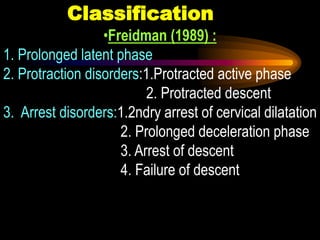
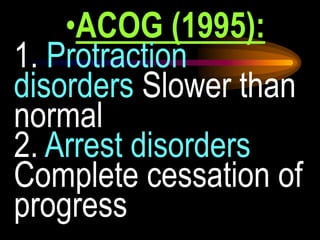
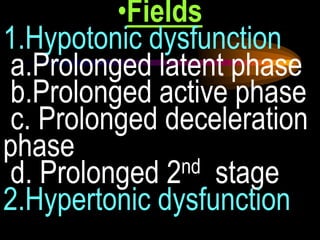
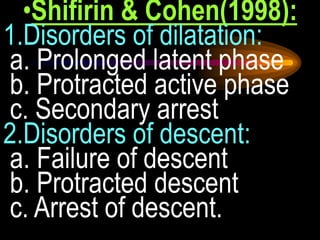
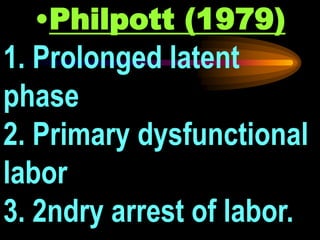
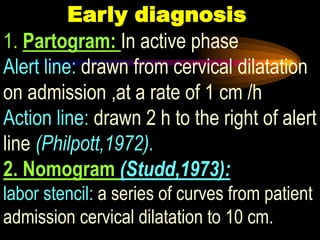
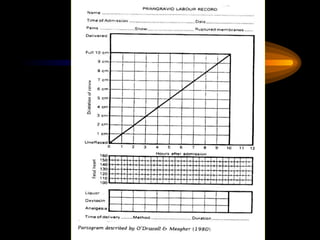
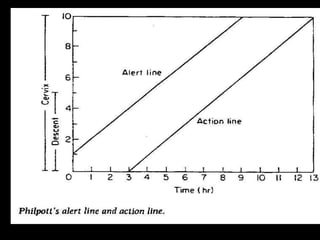
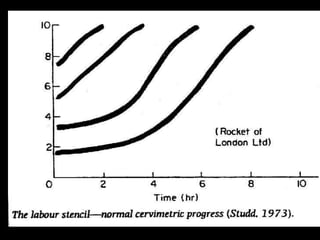
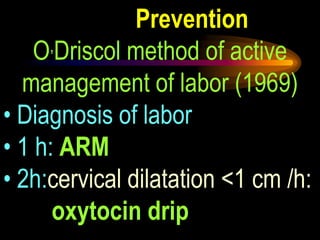
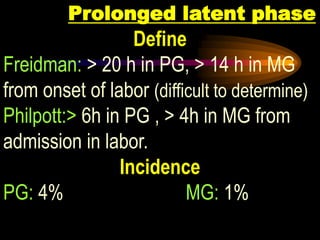
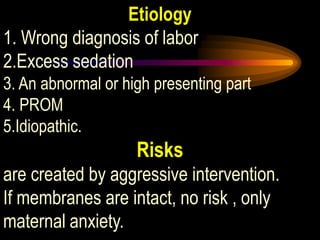
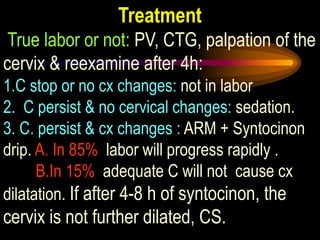
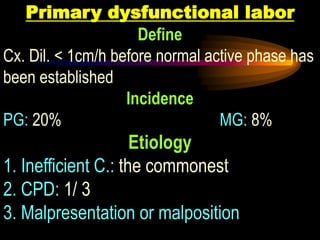
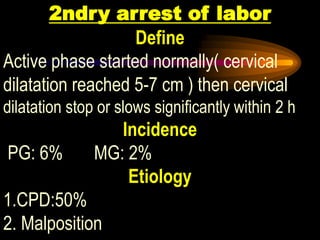
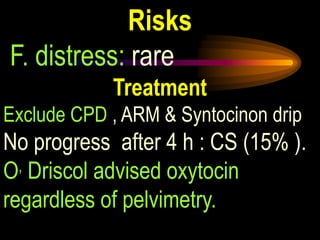
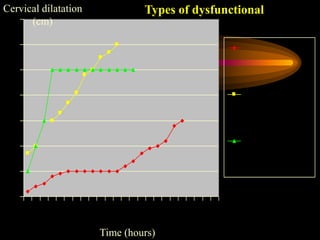
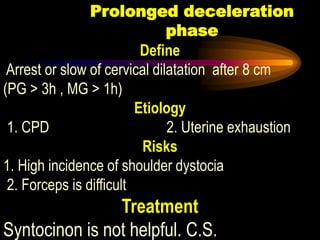
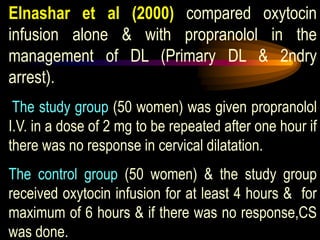
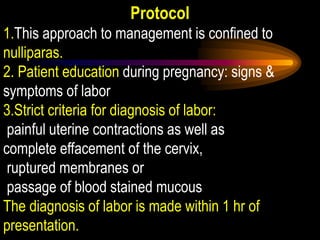
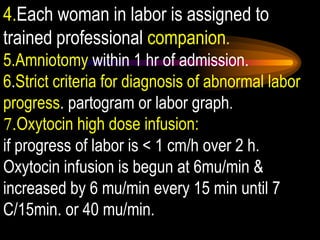
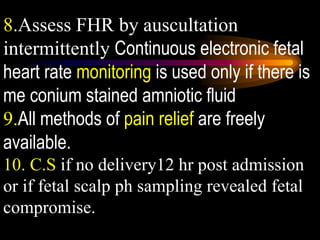
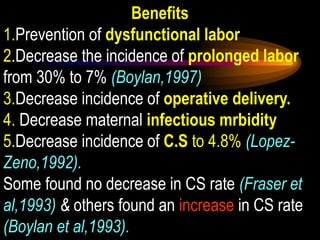
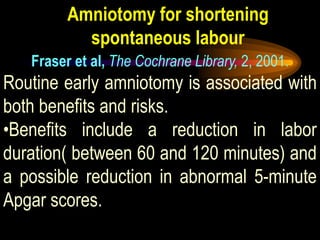
This document discusses stages of labor and dysfunctional labor. It defines the stages of labor according to Friedman and describes the latent, active and second stages. It then defines and classifies dysfunctional labor according to various authors and discusses causes, risks and treatments for specific dysfunctional labor disorders like prolonged latent phase, primary dysfunctional labor, and secondary arrest of dilation. It also discusses techniques for early diagnosis of dysfunctional labor using a partogram and methods for preventing dysfunctional labor like active management of labor developed by O'Driscoll.