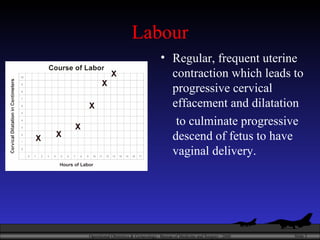
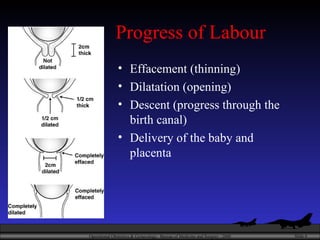
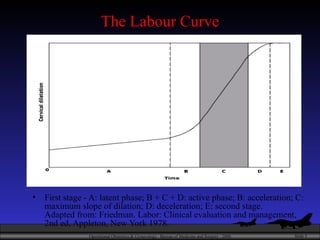
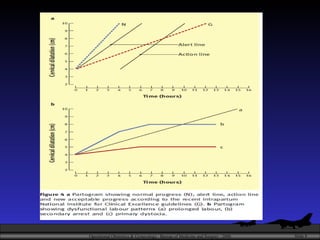
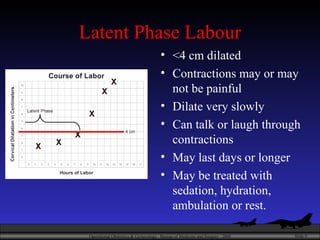
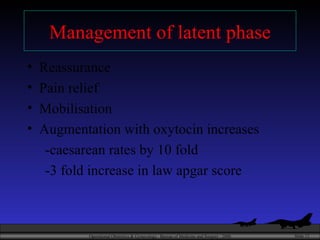
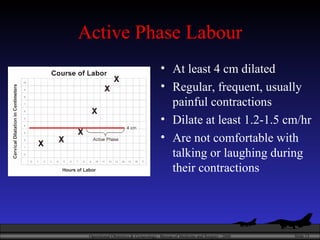
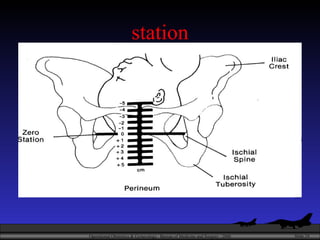
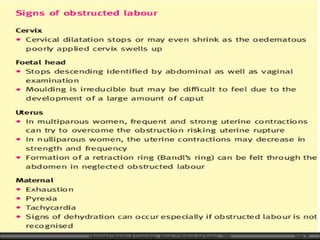
The document discusses poor progress of labor, which is a leading cause of cesarean sections, especially in first-time mothers. It defines the different stages of labor and describes disorders that can cause delayed progress, such as a prolonged latent phase, dysfunctional labor, or secondary arrest. The document provides guidance on assessing labor progress and outlines management strategies, including one-on-one care, hydration, pain relief, mobilization, amniotomy, and oxytocin augmentation when indicated to help improve labor outcomes.