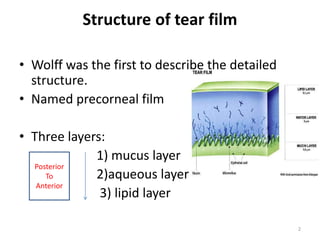
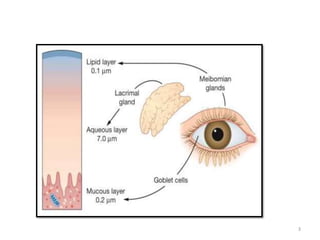
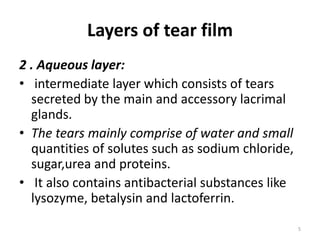
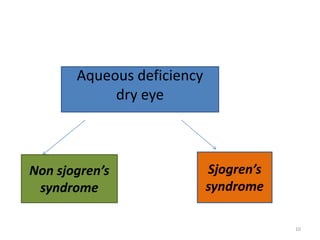
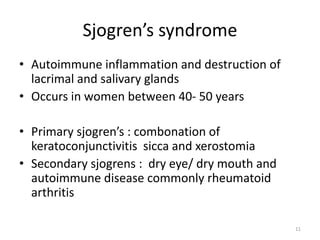
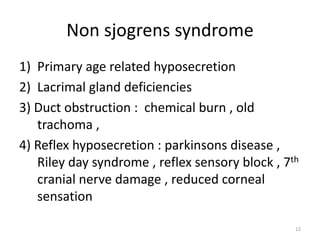
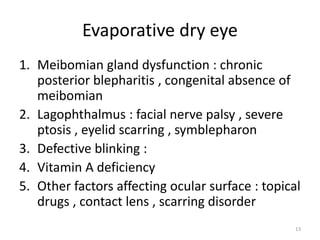
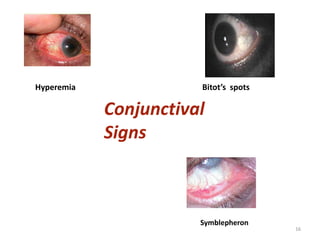
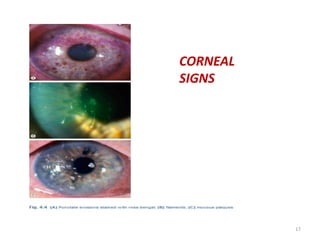
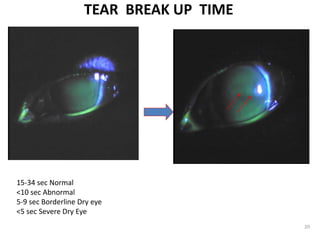
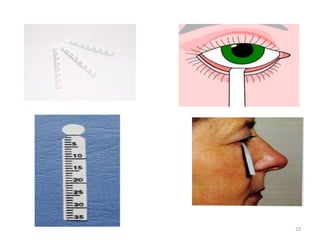
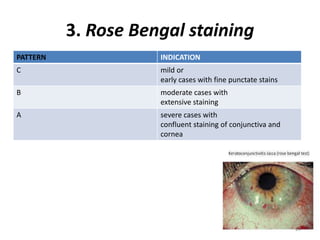
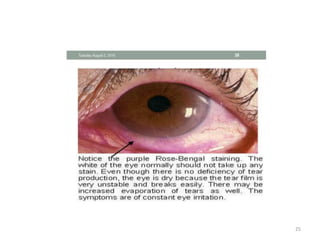
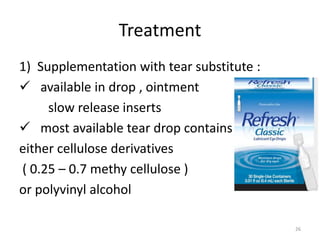
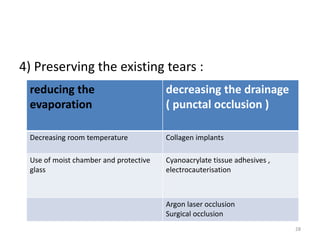
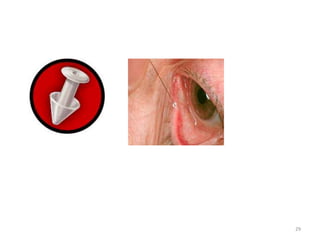
The document outlines the structure and function of the tear film, highlighting its three layers: mucus, aqueous, and lipid. It discusses dry eye conditions, their causes, clinical features, and diagnostic tests. Treatment methods for dry eye include tear substitutes, anti-inflammatory medication, and interventions to reduce tear evaporation.