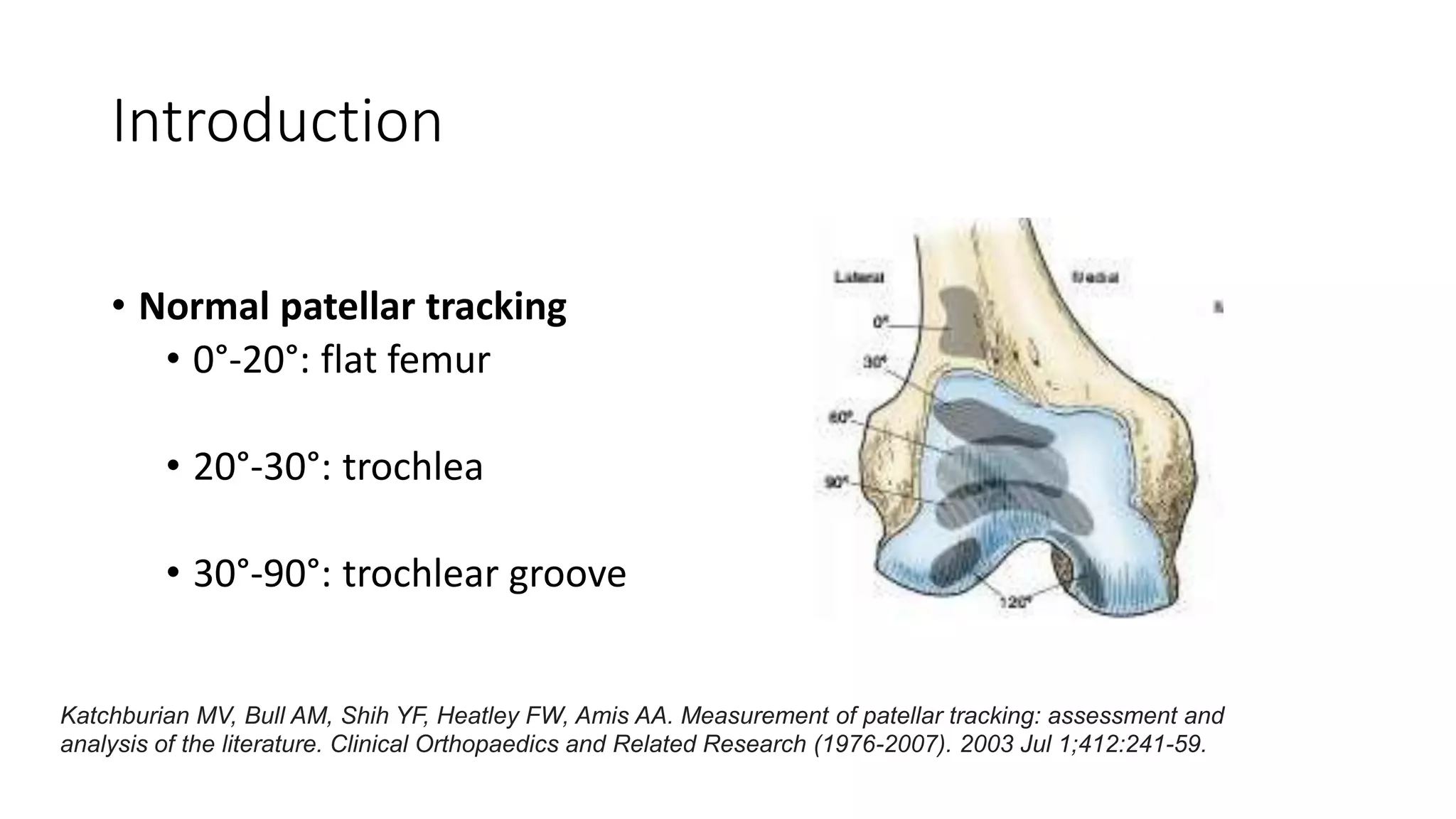
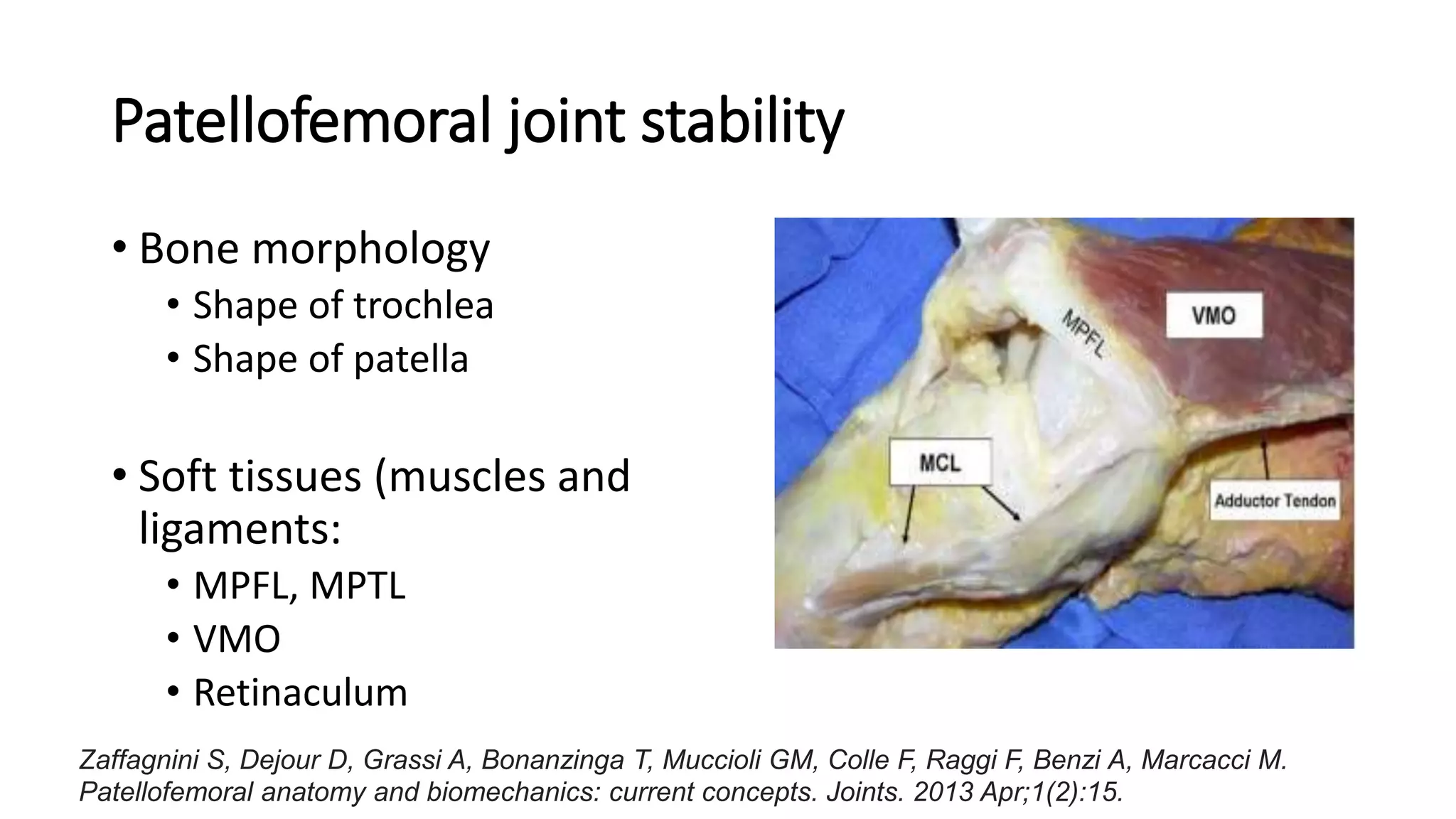
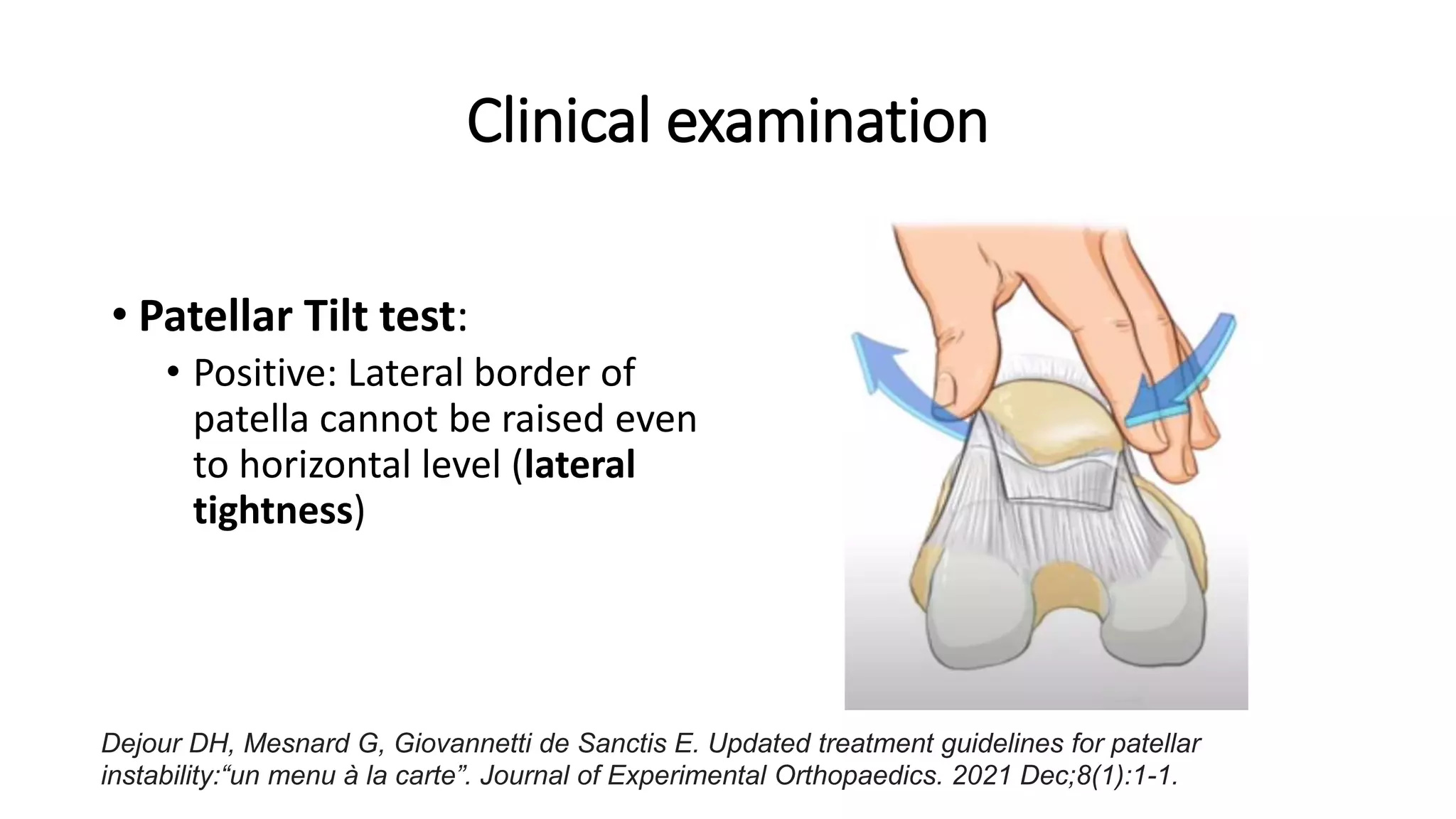
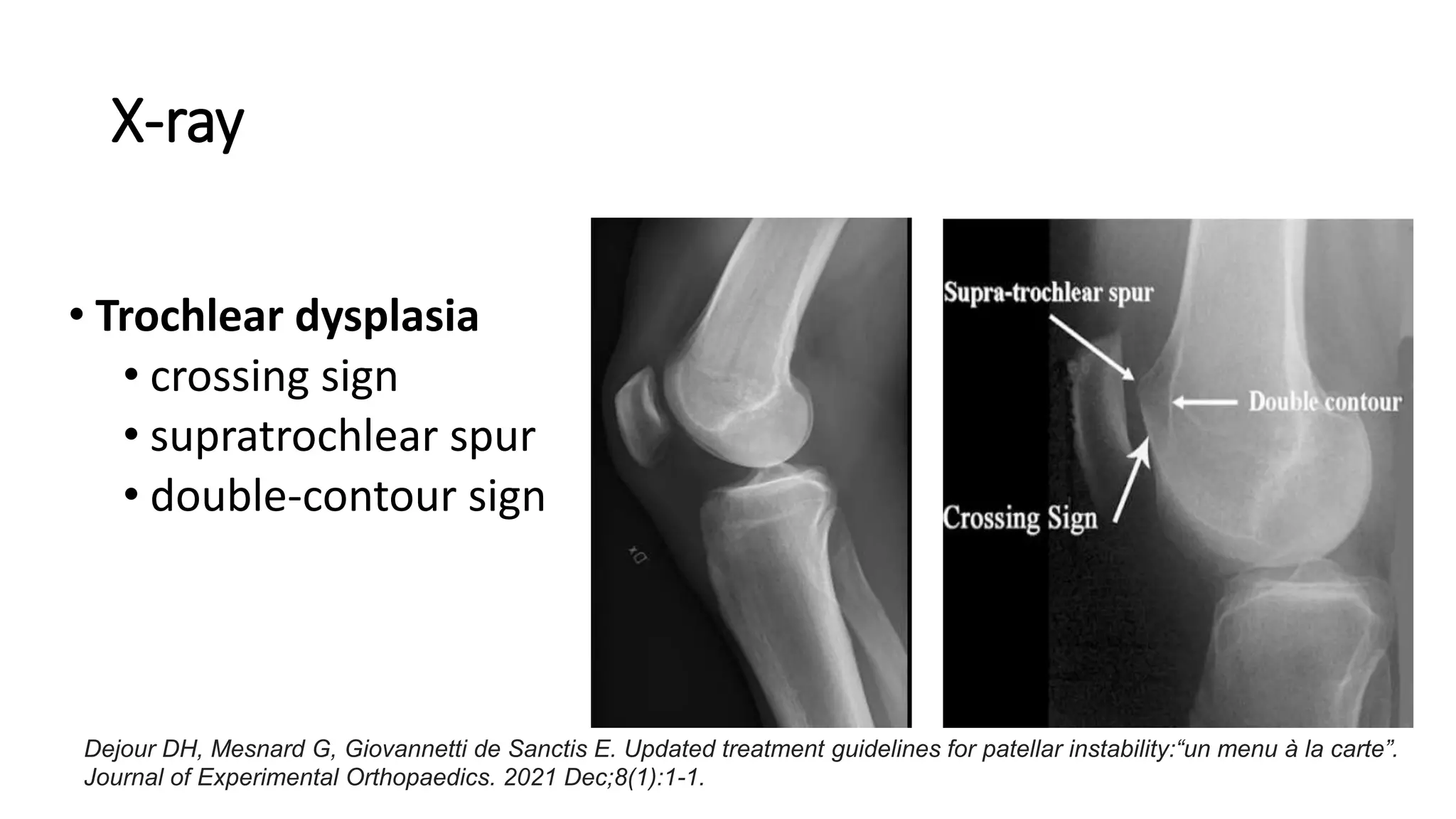
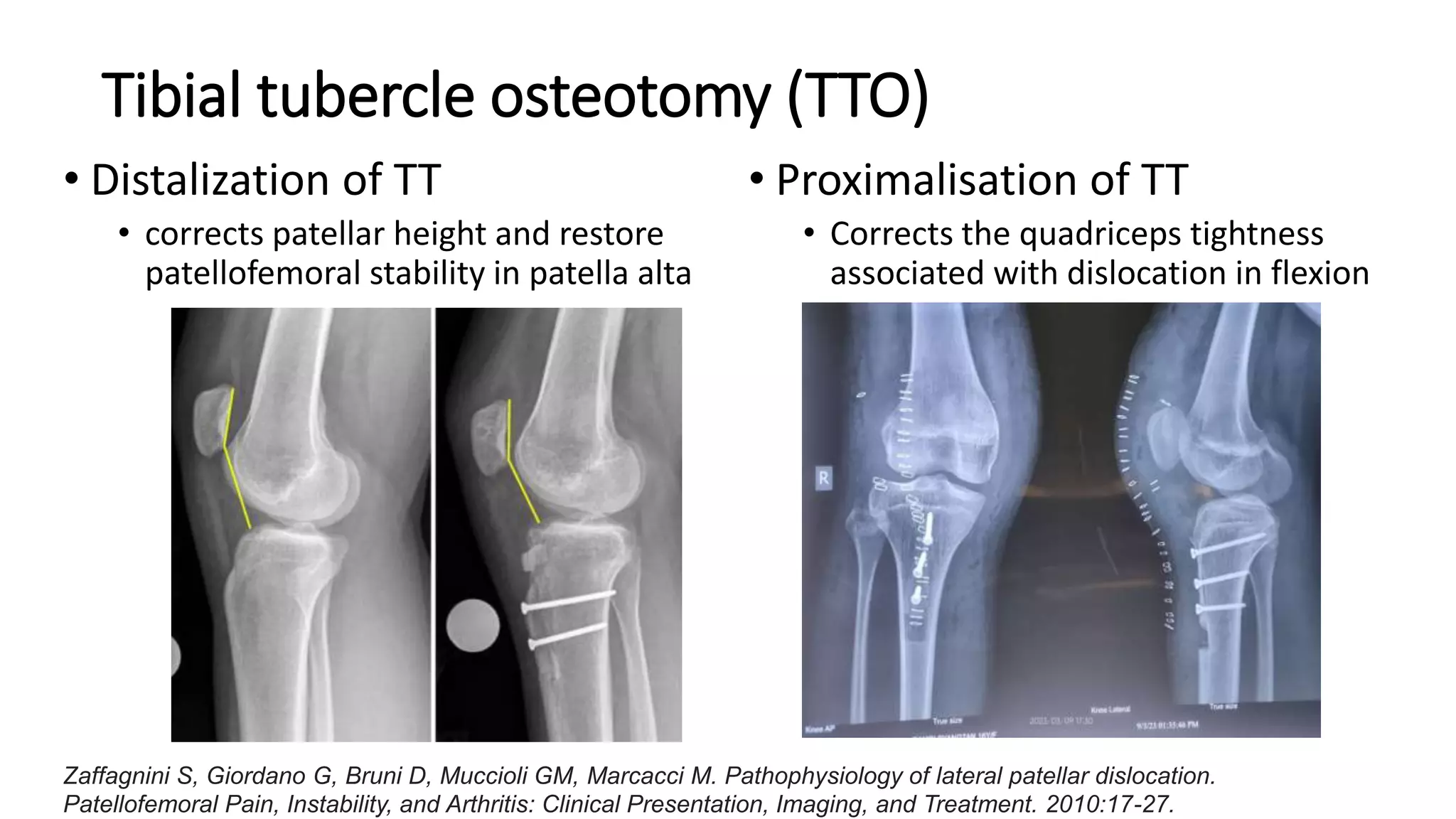
This document discusses the approach to patellofemoral instability. It begins with an introduction to normal and abnormal patellar tracking. It then covers the causes of instability which can include bone morphology issues, soft tissue problems, or abnormal alignment. The biomechanics of different pathologies like MPFL tears, patella alta, or trochlear dysplasia are described. Clinical exams and imaging studies used in evaluation are outlined. Management involves addressing the specific underlying bony or soft tissue abnormalities through procedures like MPFL reconstruction, trochleoplasty, or tibial tubercle osteotomy to restore stability.