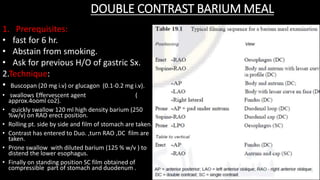
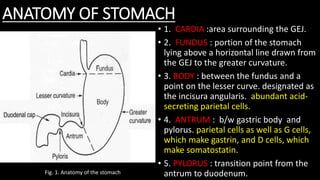
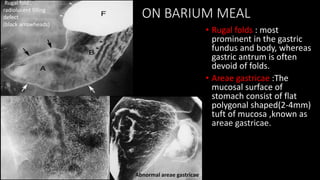
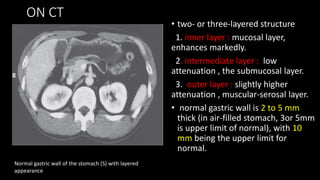
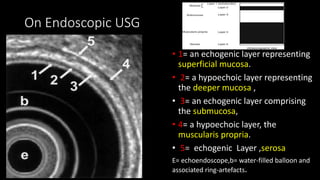
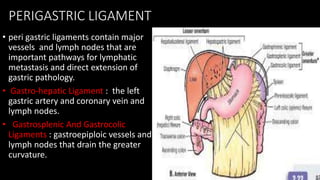
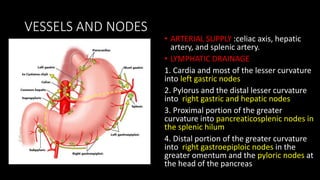
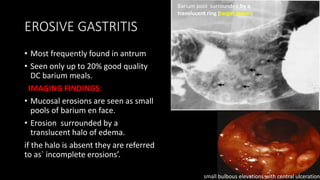
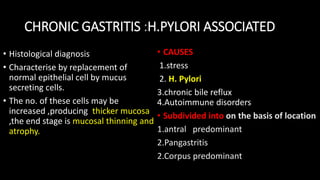
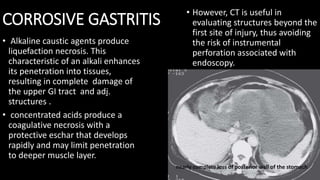
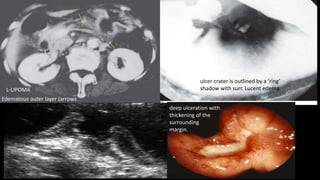
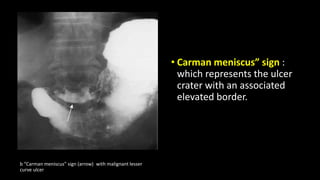
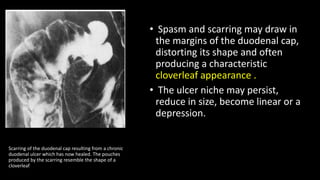
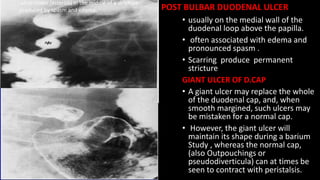
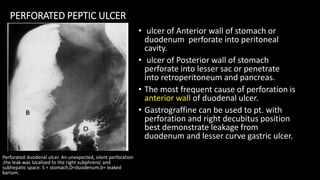
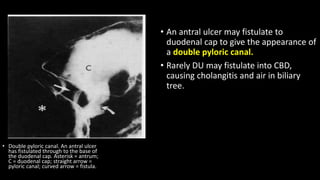
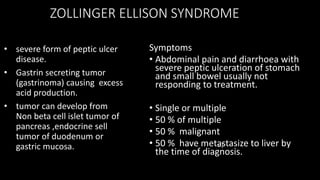
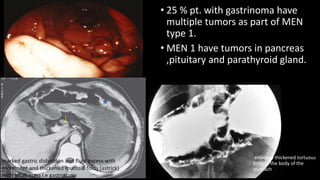
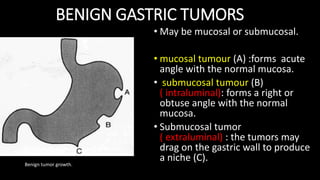
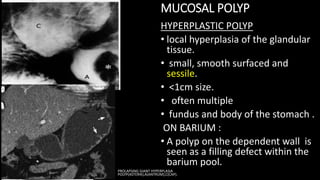
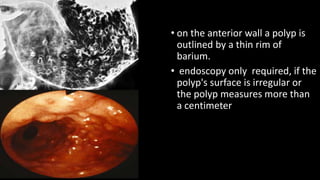
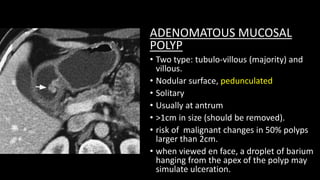
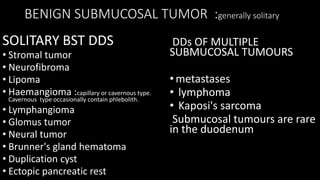
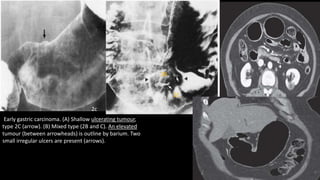
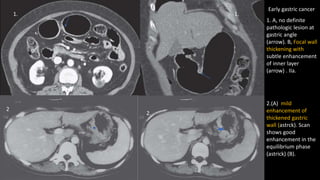
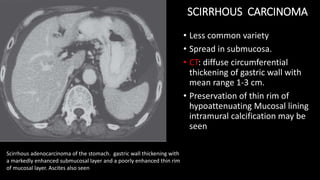
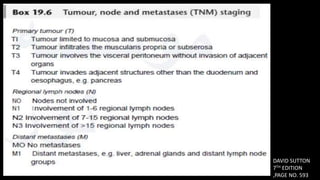
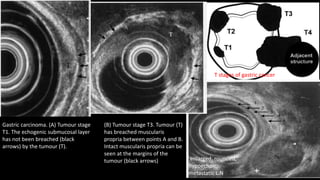
This document discusses the radiological anatomy and pathologies of the stomach. It begins with an overview of examination techniques including endoscopy, barium meal, CT, and endoscopic ultrasound. It then describes the anatomy of the stomach and surrounding structures. The main pathologies discussed are gastritis, peptic ulcer disease, neoplasms, and congenital anomalies. For inflammatory conditions like gastritis and peptic ulcers, the document outlines imaging findings and distinguishing features of different types. It similarly discusses imaging features that help differentiate benign from malignant ulcers.