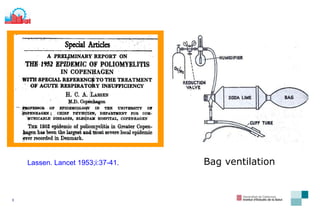
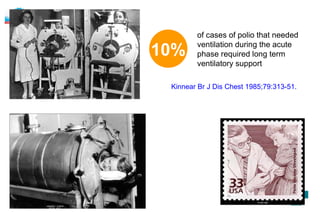
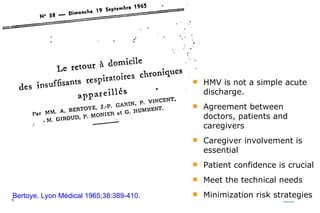
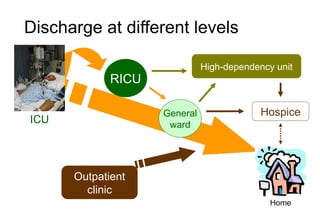
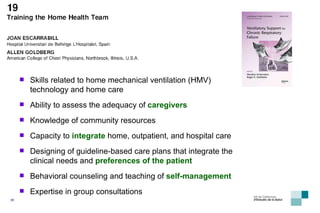
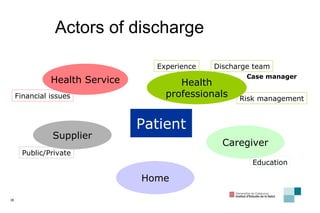
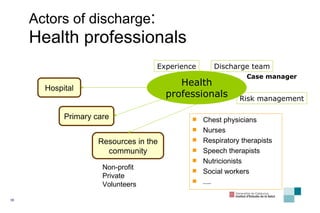
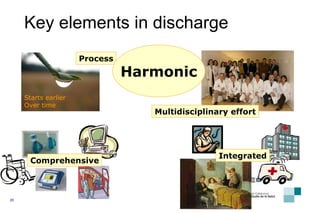
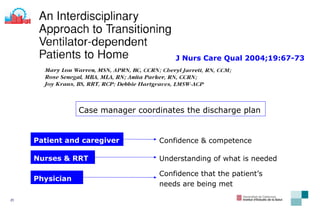
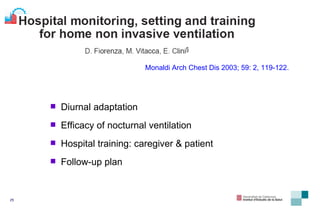
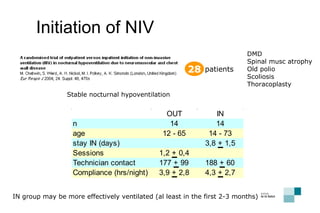
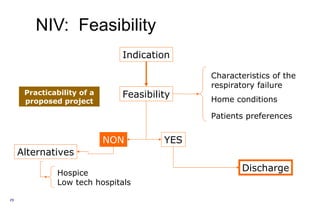
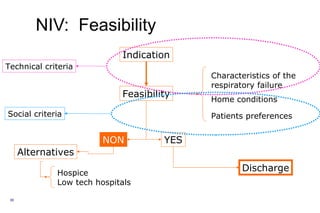
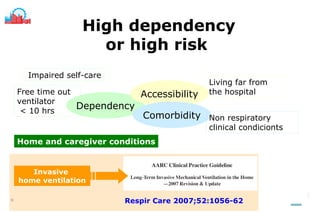
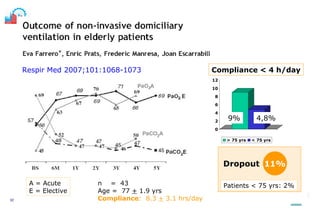
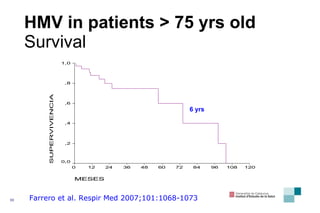
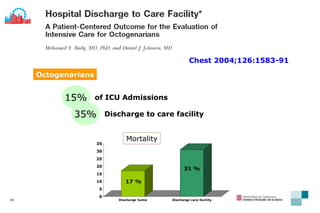
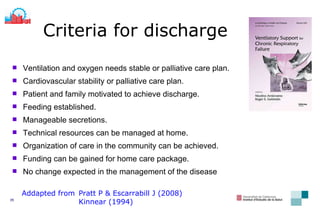
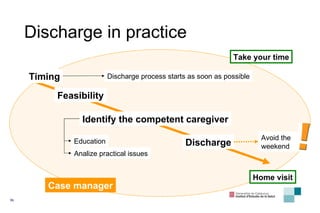
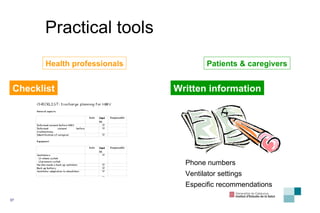
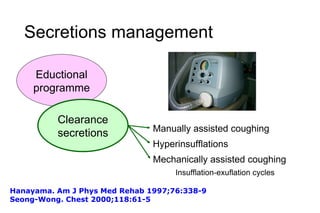
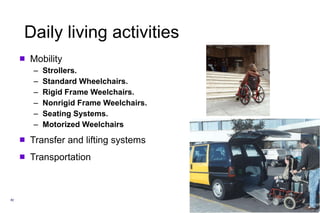
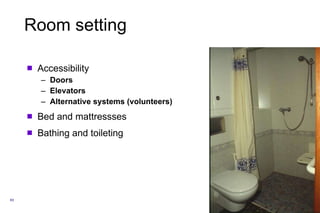
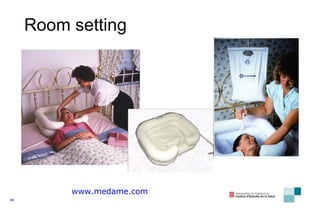
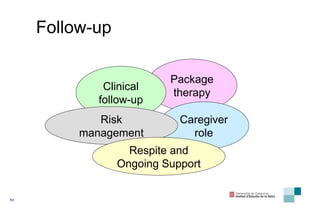
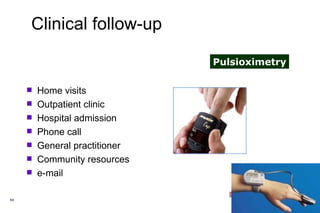
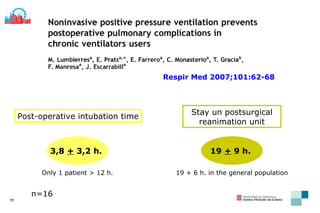
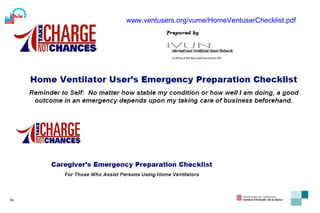
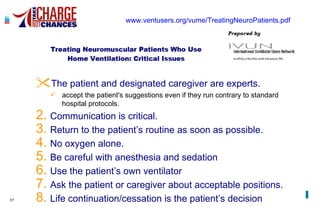
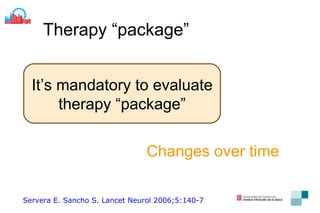
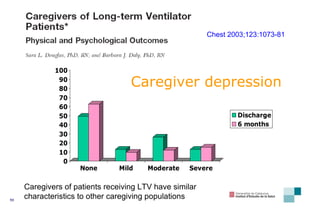
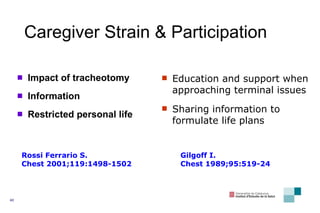
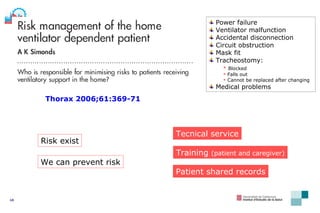
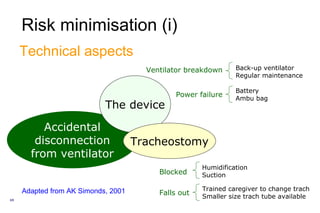
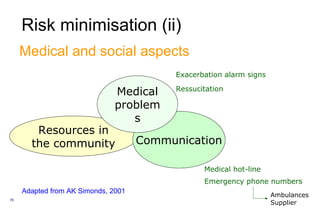
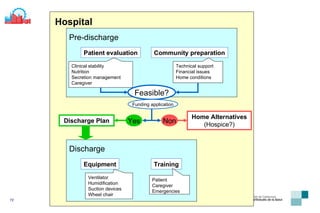
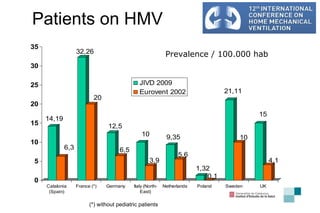
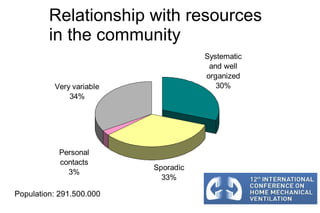
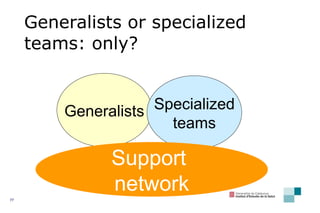
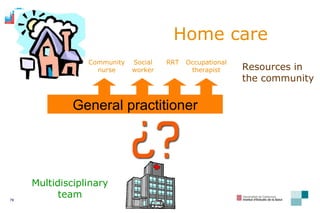
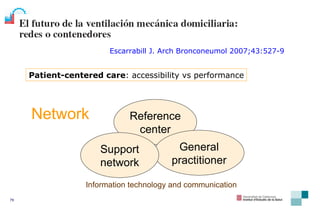
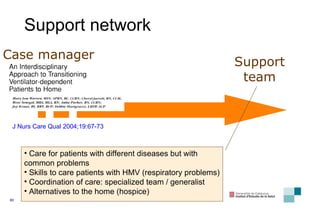
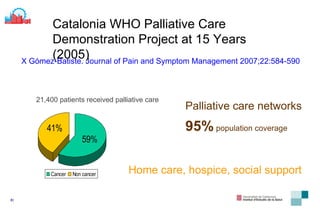
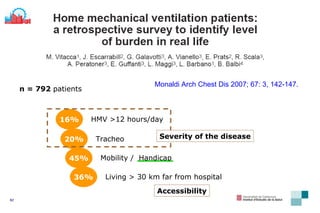
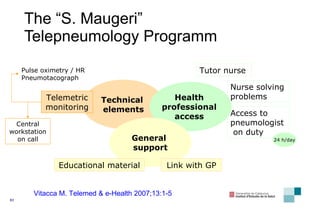
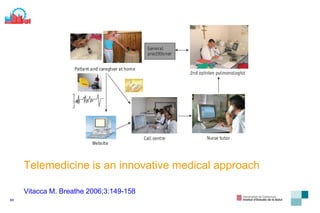
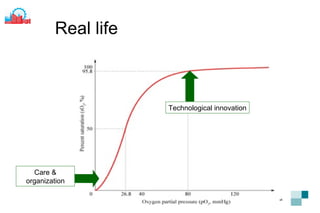
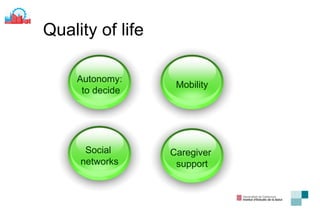
The document discusses organizing teaching and discharge management for patients requiring home mechanical ventilation (HMV). It outlines key elements of effective discharge planning including multidisciplinary teams, caregiver education and support, ensuring clinical stability and access to resources before discharge, and developing follow-up and risk management plans. Networks of specialized and generalist healthcare professionals and community resources are important to coordinate long-term care for patients after hospital discharge.
![Joan Escarrabill MD Director of Master Plan for Respiratory Diseases Institut d’Estudis de la Salut Barcelona [email_address] How to organize teaching and discharge management Vienna. September 12th 2009](https://image.slidesharecdn.com/dischargemanagementvienna09-090923123912-phpapp01/75/Discharge-Management-Vienna-09-1-2048.jpg)