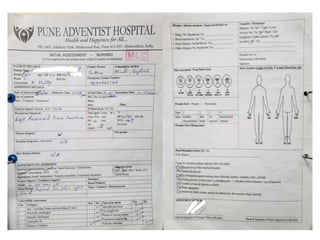
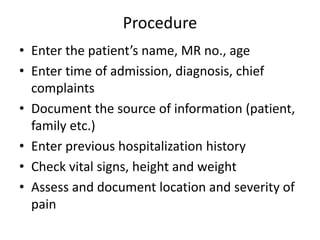
The document outlines the training procedures for nursing initial assessment at Pune Adventist Hospital, focusing on identifying patient care parameters. It details responsibilities for nurses, documentation requirements, and specific assessments needed for various bodily systems and risks, including vital signs, psychosocial factors, and nutritional status. The initial assessment must begin within 15 minutes of patient arrival and is critical for effective care planning.