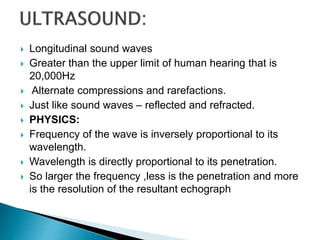
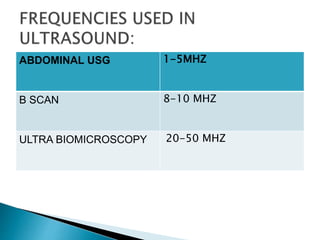
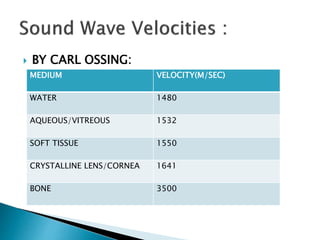
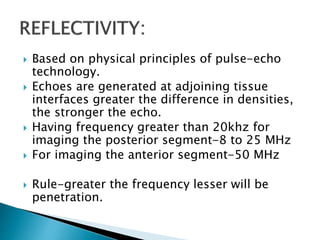
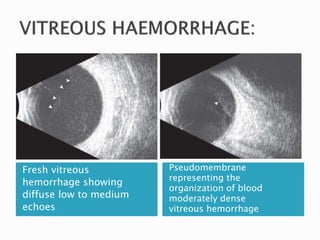
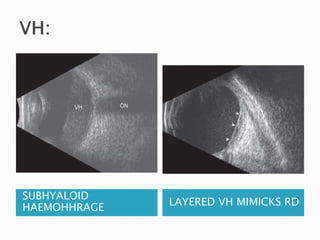
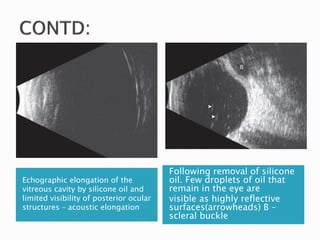
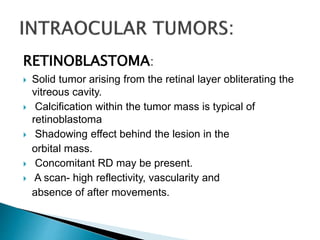
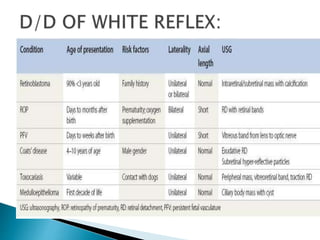
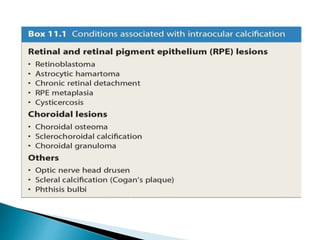
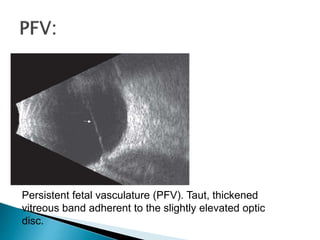
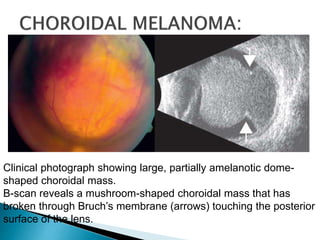
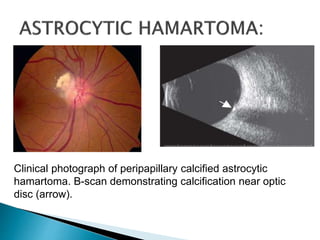
The document discusses B-scan ultrasound, providing a history of its development and describing the technical aspects and clinical applications. It notes that B-scan utilizes high frequency sound waves to produce two-dimensional images, and was first introduced in 1958. The document outlines the physics behind B-scan, describing how sound waves are reflected and the factors that determine resolution. Clinical uses mentioned include evaluating vitreous opacities, retinal detachments, and tumors.