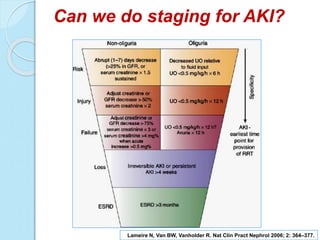
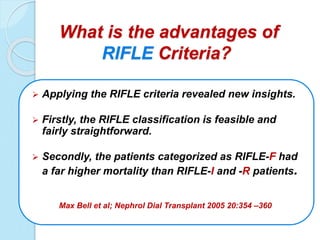
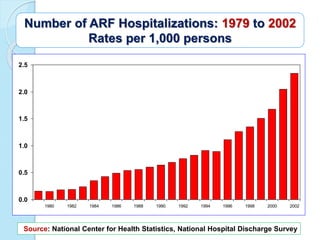
Dr. Osama El-Shahat discusses various aspects of acute kidney injury (AKI) management including staging, modalities of renal replacement therapy, and general principles. The document covers (1) staging systems like RIFLE and AKIN to classify AKI severity, (2) modalities like intermittent hemodialysis, slow continuous ultrafiltration, and continuous renal replacement therapy, and (3) general guidelines around initiating renal replacement therapy, vascular access, solutions, anticoagulation, and dose of therapy. The overall message is that managing AKI requires an individualized approach and more high-quality research is still needed.