CRRT and AKI
- Continuous renal replacement therapy (CRRT) is a treatment for acute kidney injury (AKI) that can remove fluid and waste products from patients who are hemodynamically unstable.
- CRRT was developed in the 1970s-1980s and uses an extracorporeal blood pump and catheter to continuously filter blood outside the body.
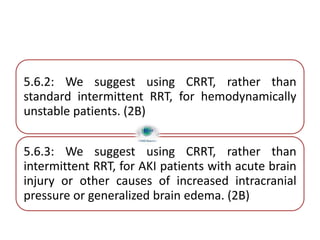
- The choice of CRRT or intermittent dialysis depends on the patient's condition and stability, with CRRT often preferred for unstable patients with fluid overload or brain injury.
- Proper nursing management before, during, and after CRRT is crucial and includes assessments, monitoring, preventing mechanical issues, and managing antico