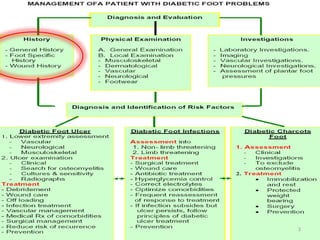
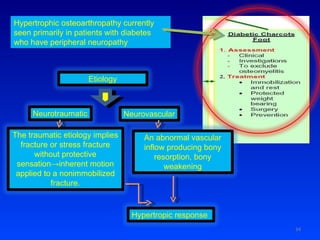
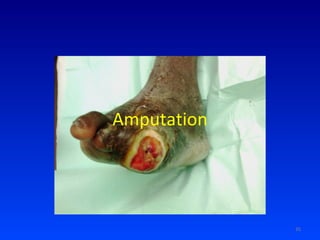
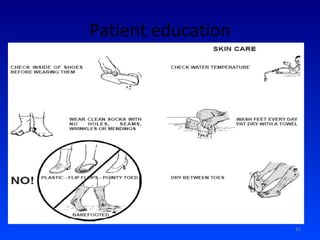
The document discusses the evaluation and treatment of diabetic foot problems. It outlines the importance of assessing a patient's medical history, examining the foot and lower limb for issues like neuropathy, vascular disease and foot deformities, and investigating for conditions like infection. Treatment involves wound care, reducing pressure on ulcers through offloading techniques, managing infection, improving vascular issues, and potentially surgical interventions like debridement or amputation.