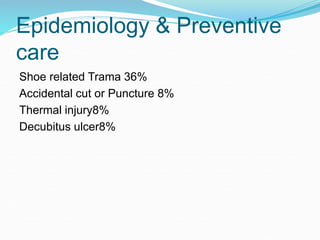
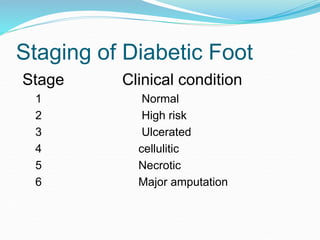
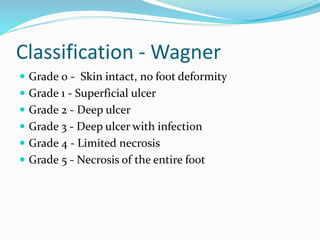
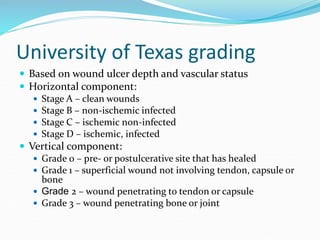
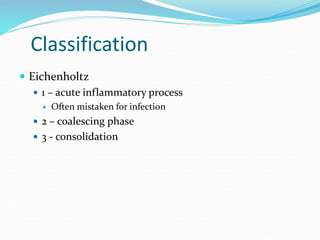
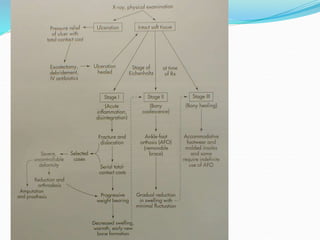
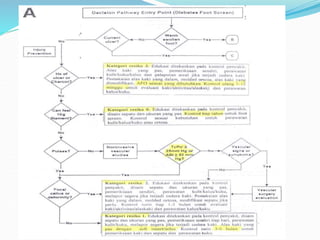
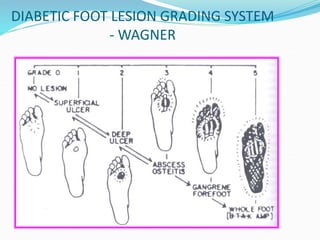
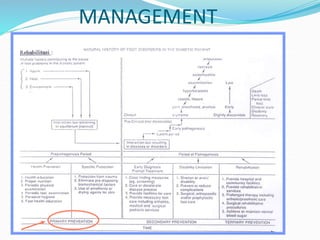
This document provides information on diabetic foot, including its definition, epidemiology, pathophysiology, risk factors, patient evaluation, classification, and treatment modalities. Some key points include:
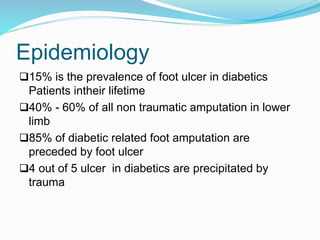
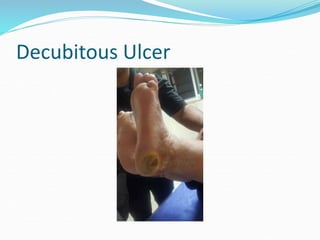
- Diabetic foot is defined as foot pathology resulting from diabetes or its complications and affects around 15% of diabetics in their lifetime.
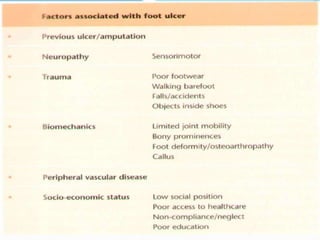
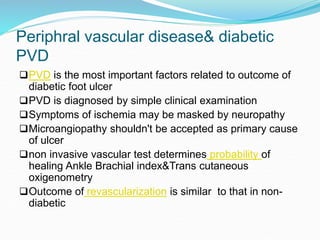
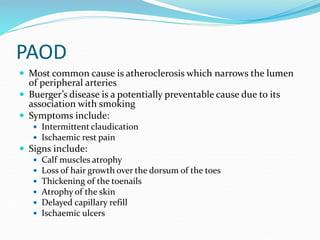
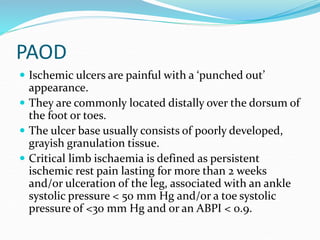
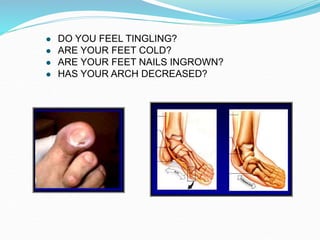
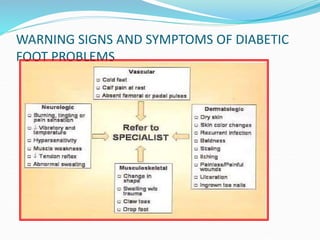
- Risk factors for diabetic foot include peripheral neuropathy, peripheral arterial disease, foot deformities, and poor glycemic control.
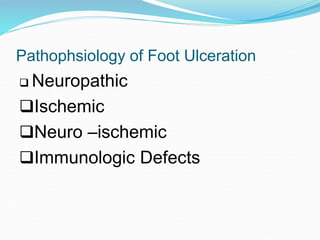
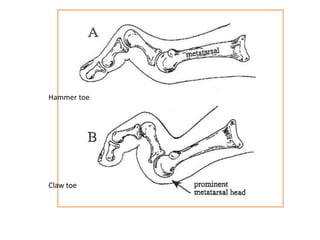
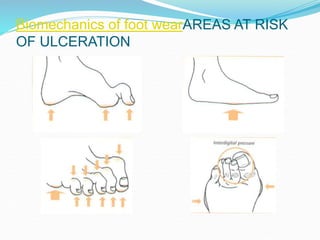
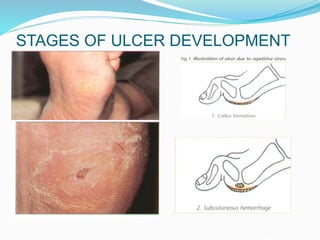
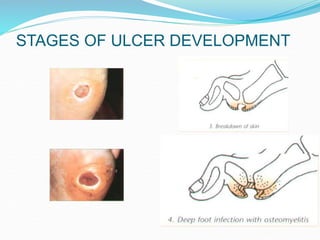
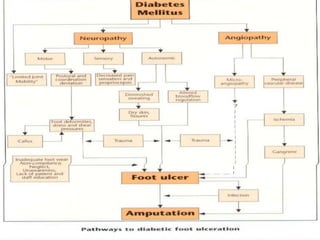
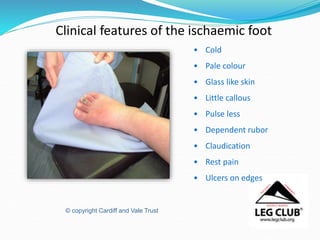
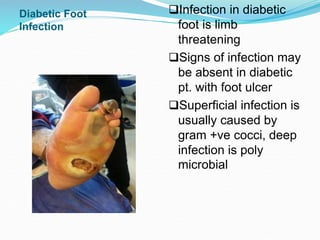
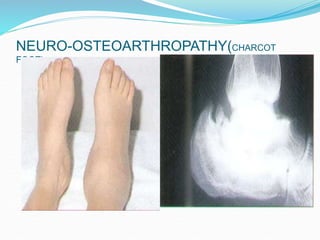
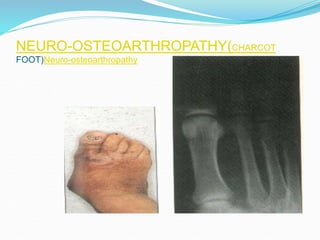
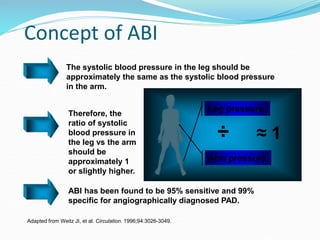
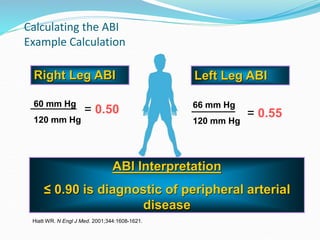
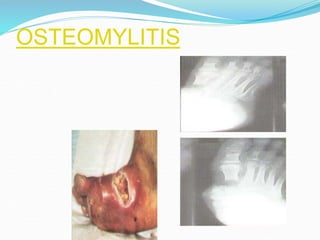
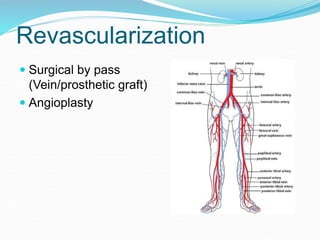
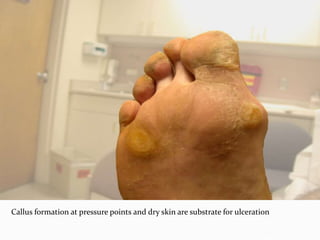
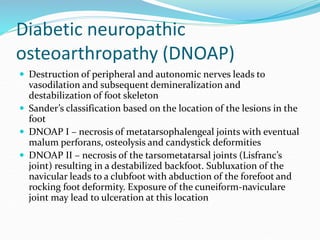
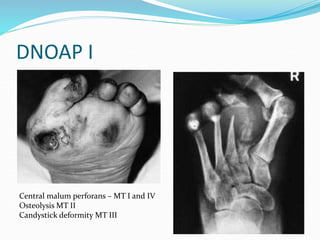
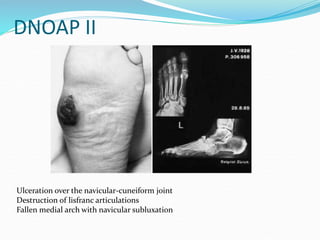
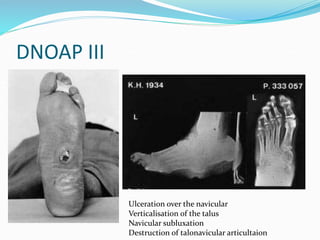
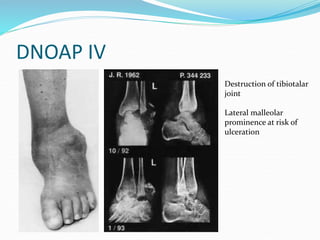
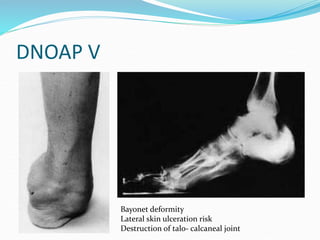
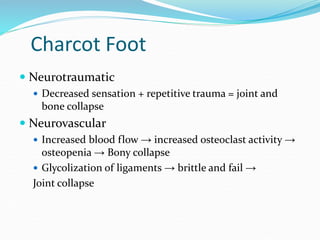
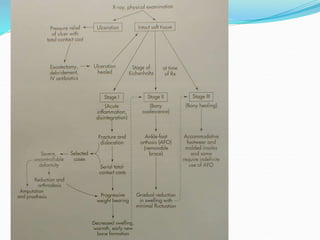
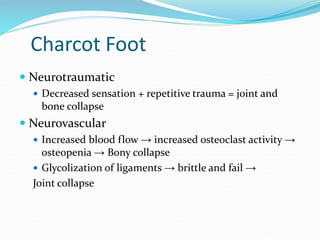
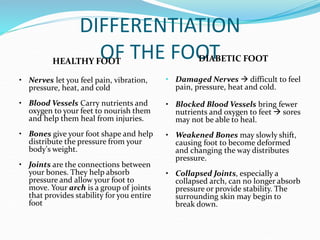
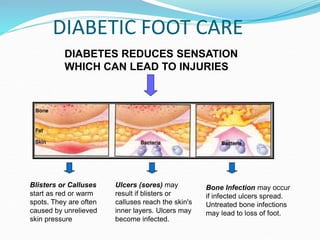
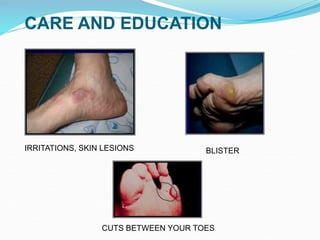
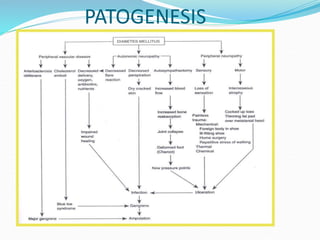
- Pathophysiology involves diabetic angiopathy reducing blood supply, neuropathy damaging sensation, and osteoarthropathy causing deformities - all of which can lead to foot ulcers and infection.
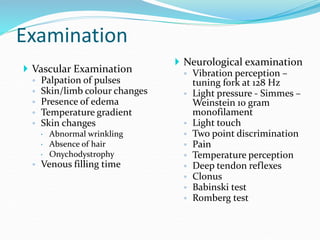
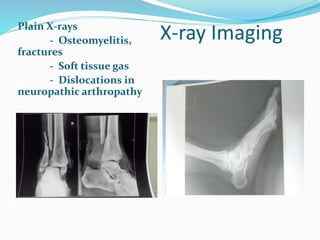
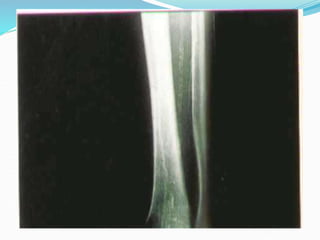
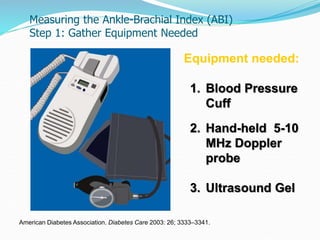
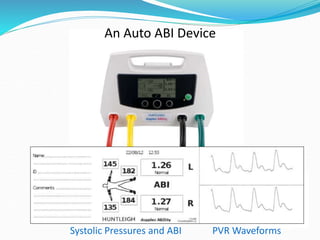
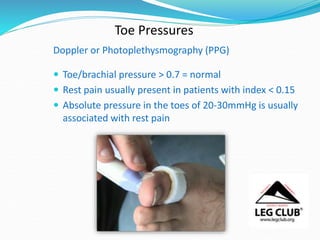
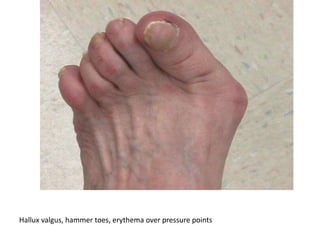
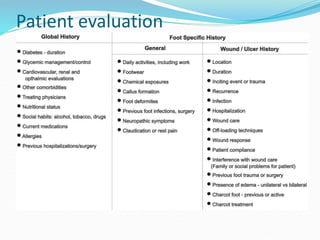
- Patient evaluation includes assessment of dermatological features, musculoskeletal structure