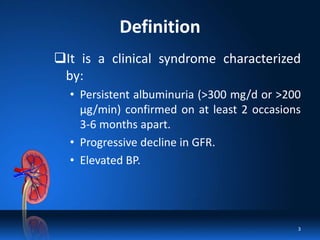
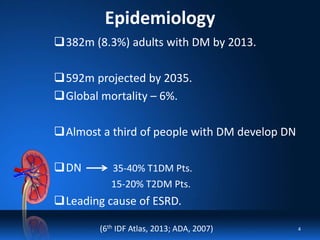
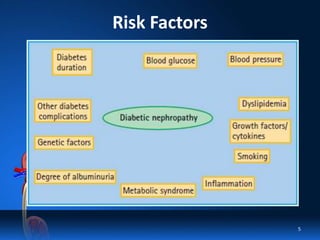
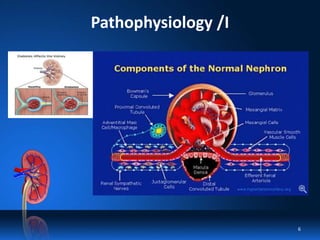
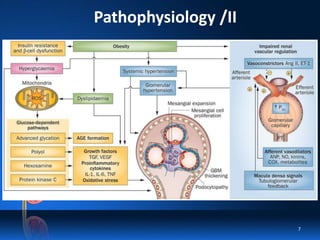
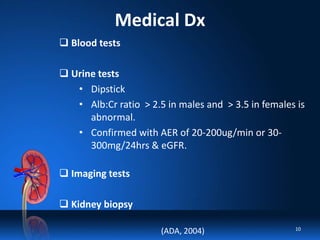
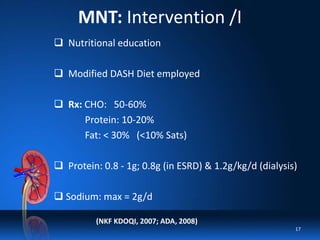
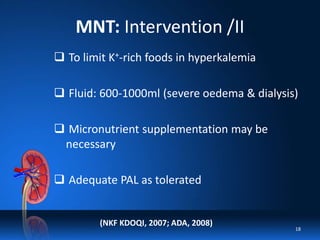
Diabetic nephropathy is a clinical syndrome characterized by persistent albuminuria and a progressive decline in kidney function. It is the leading cause of end-stage renal disease. Risk factors include poor blood glucose control, high blood pressure, smoking, and family history of kidney disease. The pathophysiology involves changes in the kidney's small blood vessels caused by high blood glucose levels over time. Common signs and symptoms include edema, trouble sleeping, weakness, and itching skin. Medical diagnosis involves blood and urine tests to assess kidney function and detect albuminuria. Management focuses on tight blood glucose and blood pressure control through medication, diet, exercise and lifestyle changes to slow disease progression and prevent complications like heart disease.