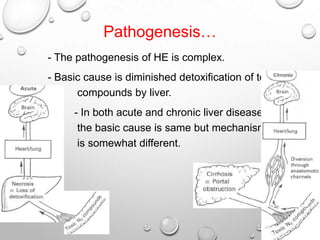
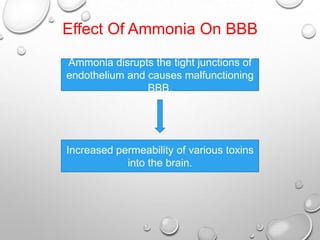
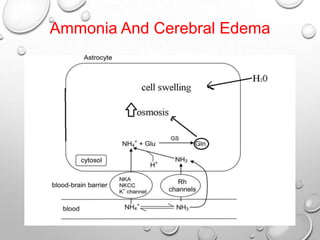
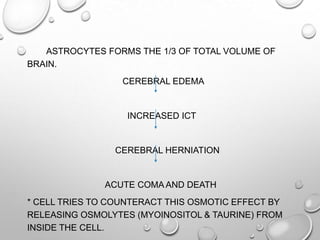
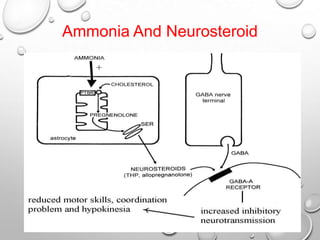
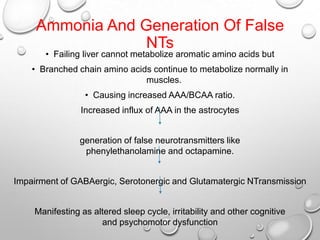
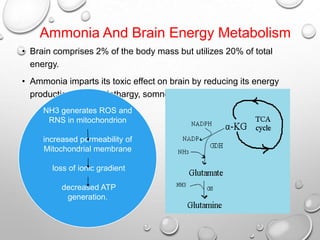
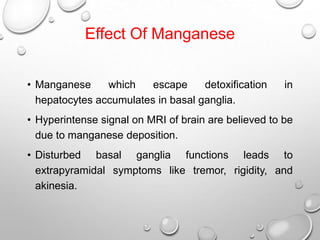
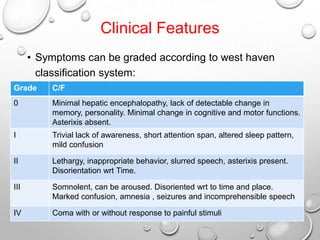
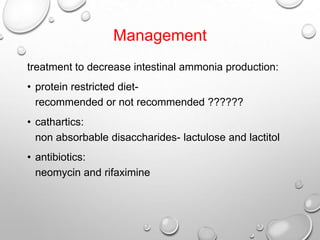
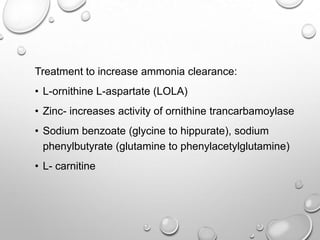
Hepatic encephalopathy is a neuropsychiatric syndrome caused by liver dysfunction and the buildup of toxins such as ammonia that are normally processed by the liver. Symptoms range from mild confusion to coma and death. Ammonia disrupts the blood-brain barrier and causes cerebral edema, increased intracranial pressure, and reduced brain energy metabolism. Other toxins like manganese, mercaptans, and false neurotransmitters also contribute. Treatment focuses on reducing ammonia production in the gut and increasing ammonia clearance from the blood and brain.