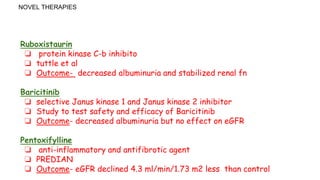
DKD is a leading cause of ESRD in the US, affecting 30-40% of those with diabetes. Poor glycemic control and hypertension are major risk factors for developing and progressing DKD. Clinical trials have shown that intensive control of blood glucose and blood pressure can delay and prevent kidney disease. New drugs targeting the kidney are showing promise in reducing albuminuria and slowing kidney function decline in DKD patients.