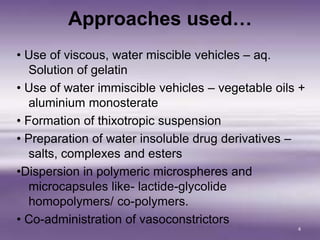
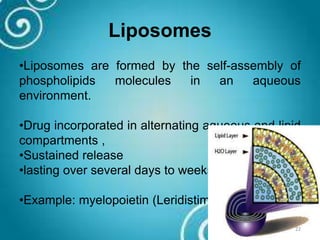
This document presents information on parenteral depot systems for long acting drug formulations. It discusses various approaches for controlled drug release including the use of viscous vehicles, polymeric microspheres, and drug derivatives. Common polymers used in depots are described as well as desirable characteristics. The main types of depot formulations are discussed - dissolution controlled, adsorption, encapsulation, and esterification. Examples of specific long acting preparations are provided for antibiotics, insulin, vitamin B12, and contraceptives. Evaluation methods and the development of depots are outlined.