This document provides information about dementia, including:
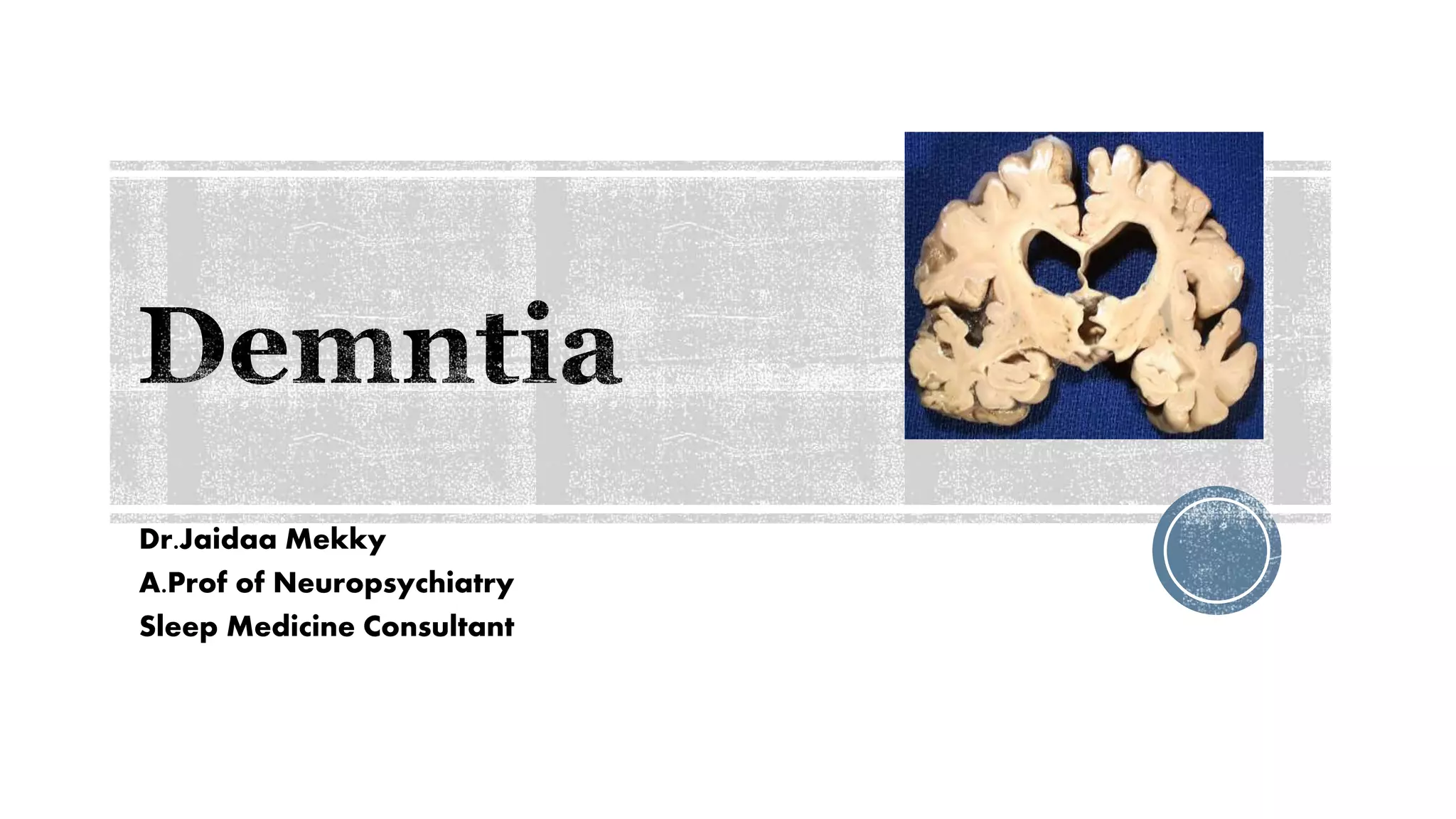
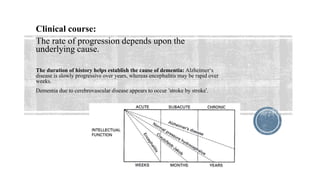
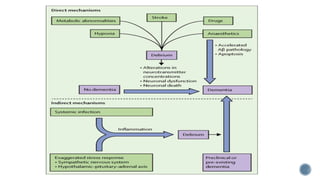
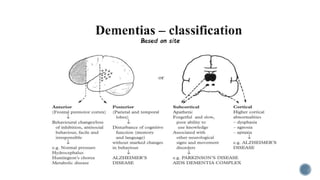
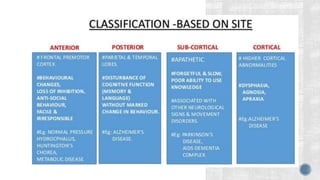
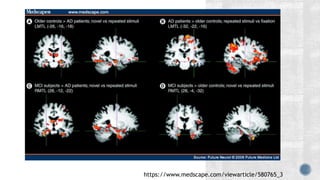
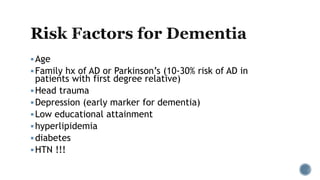
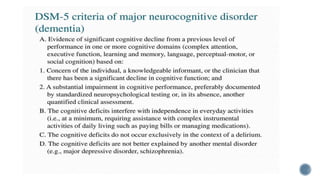
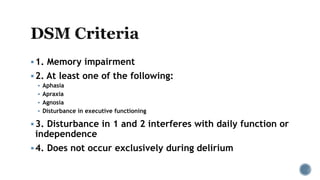
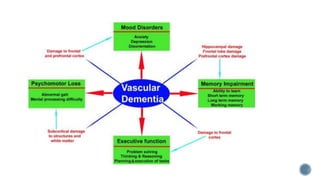
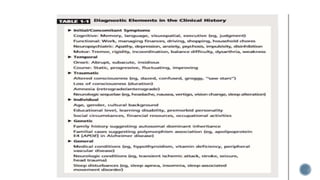
1. Dementia is characterized by progressive deterioration of intellect, behavior, and personality due to diffuse brain disease, especially affecting the cortex and hippocampus. Memory impairment is required for diagnosis.
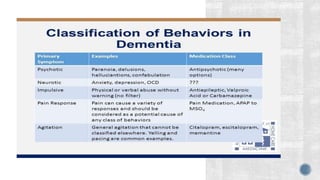
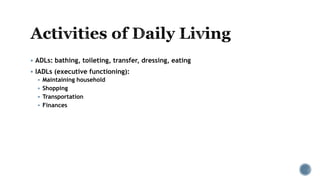
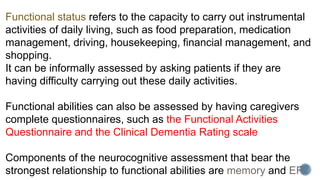
2. Symptoms include memory loss, abnormal behavior, intellectual decline, mood changes, and difficulty with daily tasks. Insight is initially retained but lost over time.
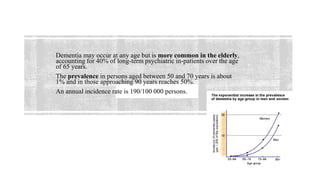
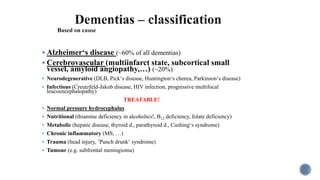
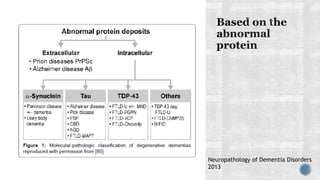
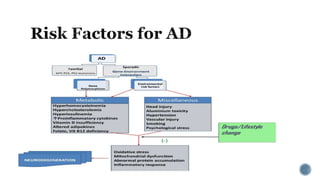
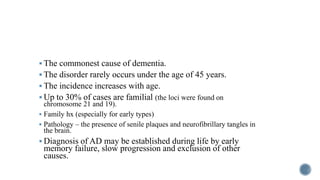
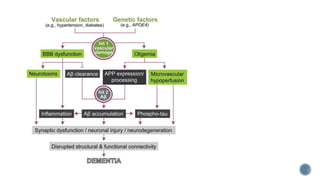
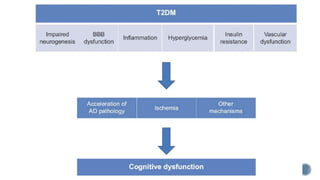
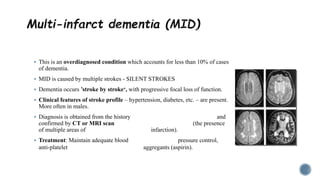
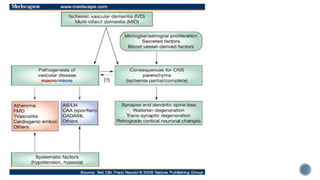
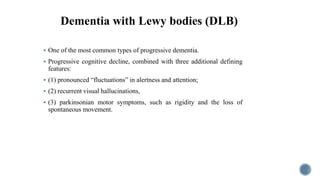
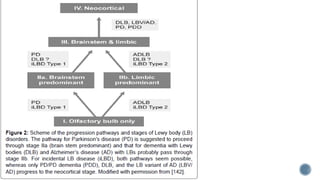
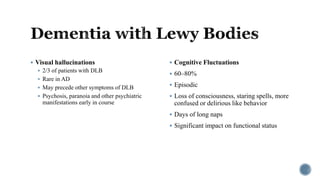
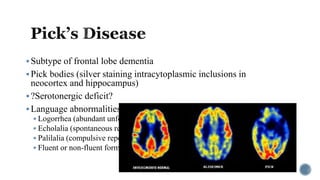
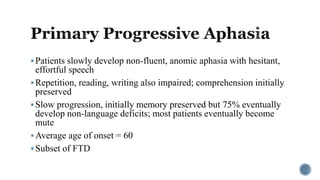
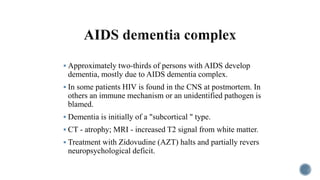
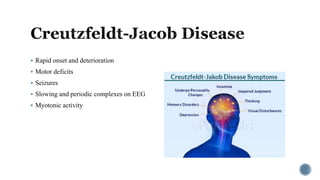
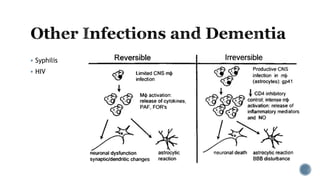
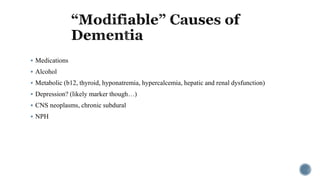
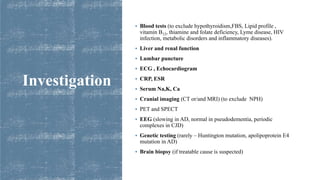
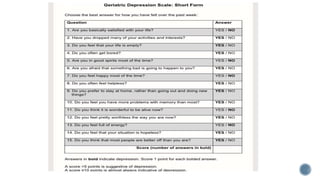
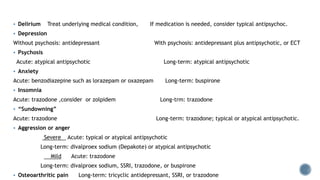
3. Causes of dementia include Alzheimer's disease (60% of cases), cerebrovascular disease, neurodegenerative diseases, infections, head injuries, and tumors. Dementia must be distinguished from delirium and depression.