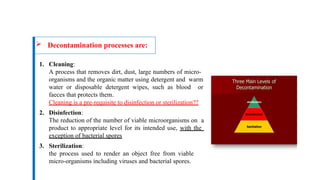
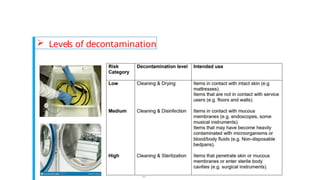
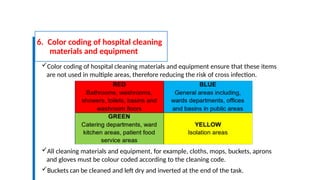
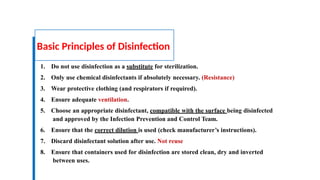
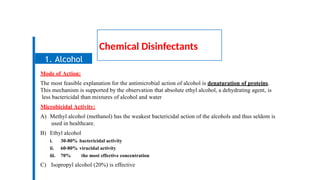
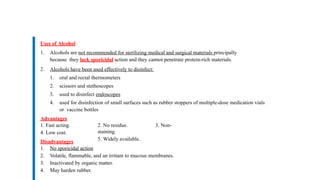
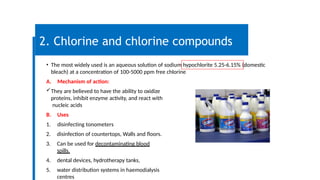
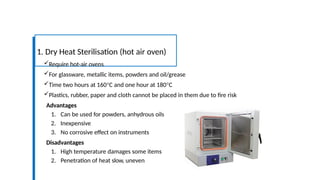
This document provides an overview of decontamination methods critical for infection prevention control (IPC) in healthcare settings. It covers three main processes: cleaning, disinfection, and sterilization, detailing various techniques, materials, and safety measures required for effective decontamination. The emphasis is on the importance of properly cleaning and disinfecting equipment to prevent the spread of infections and ensure safety for both patients and staff.