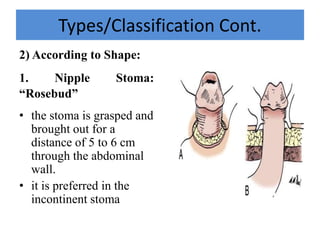
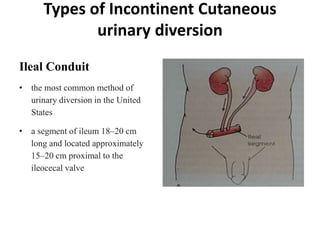
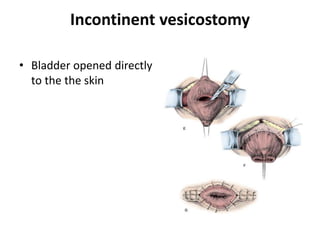
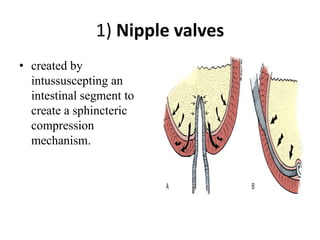
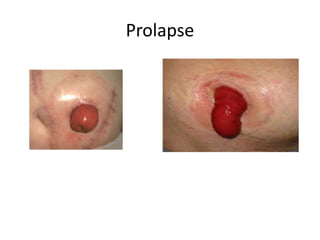
This document describes cutaneous urinary diversion, which involves creating an artificial opening in the skin for urinary elimination when the bladder has been removed or damaged. It defines urinary diversion and lists indications. It describes types of diversions based on elevation from the skin surface and shape. It discusses incontinent diversions like ileal conduits and continent diversions using techniques like Mitrofanoff appendicovesicostomy. Early and late complications of stomas are outlined, including ischemia, hemorrhage, stenosis, prolapse, hernia, and skin issues. Management strategies are provided for various complications that may arise.