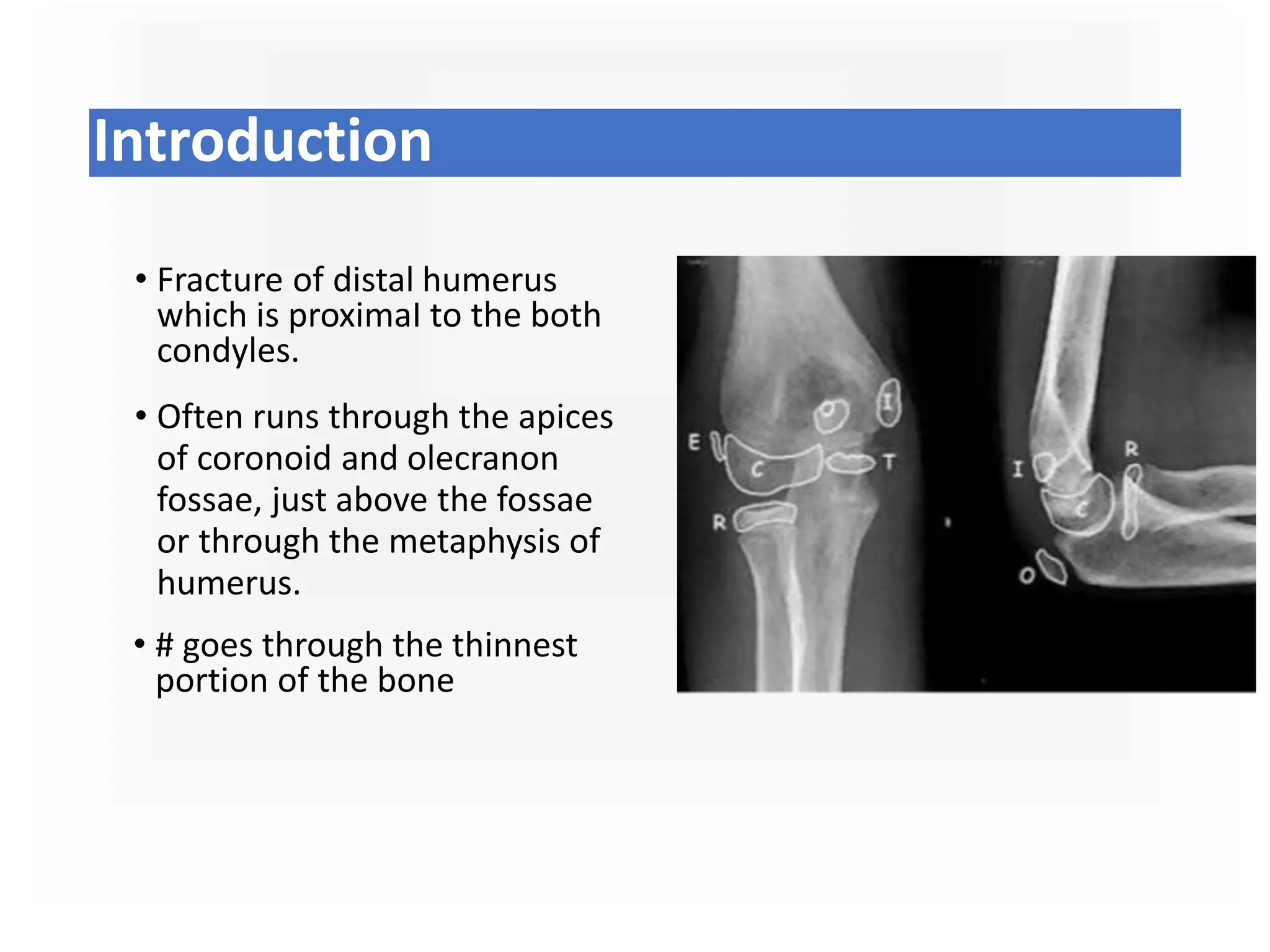
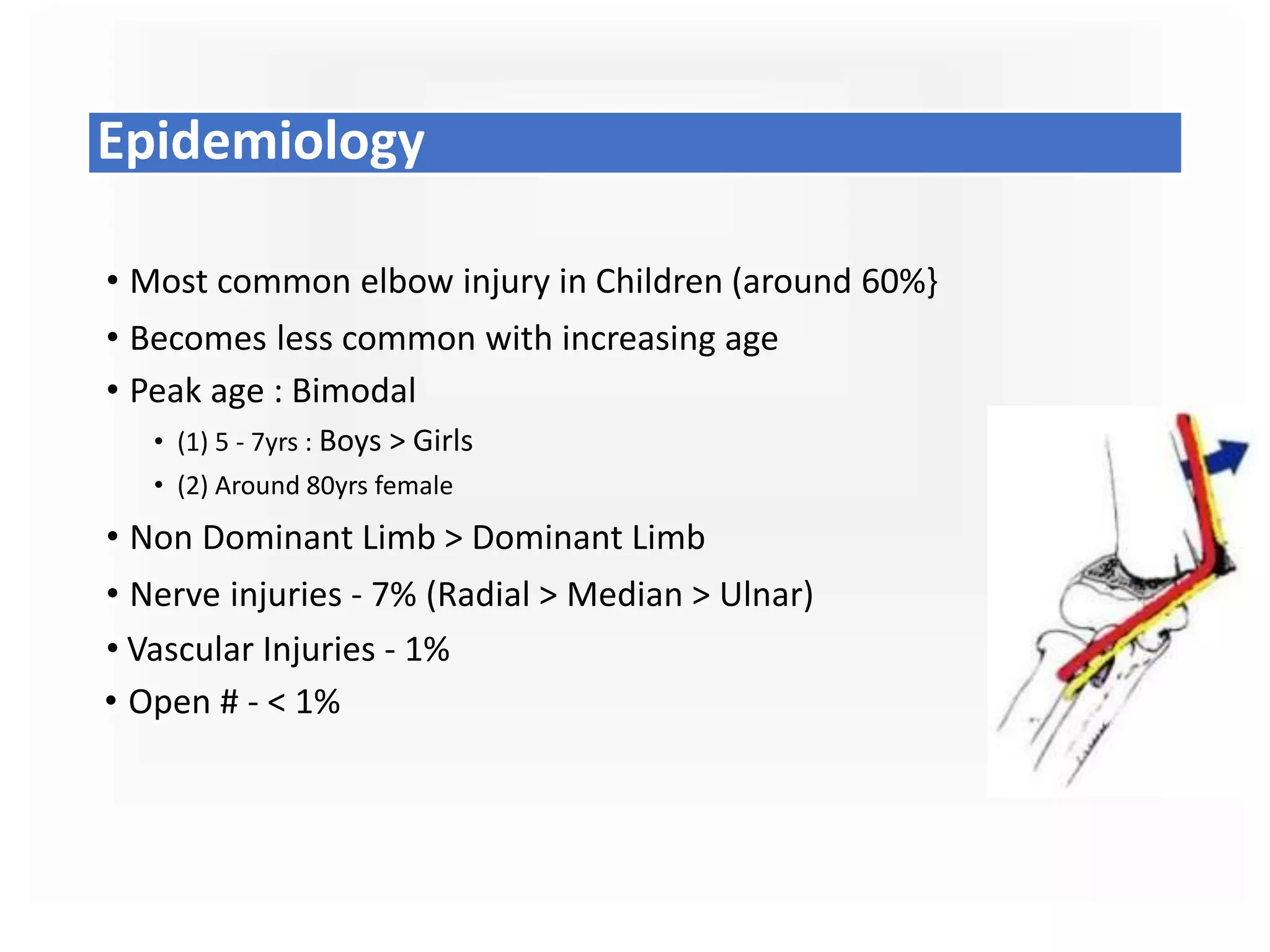
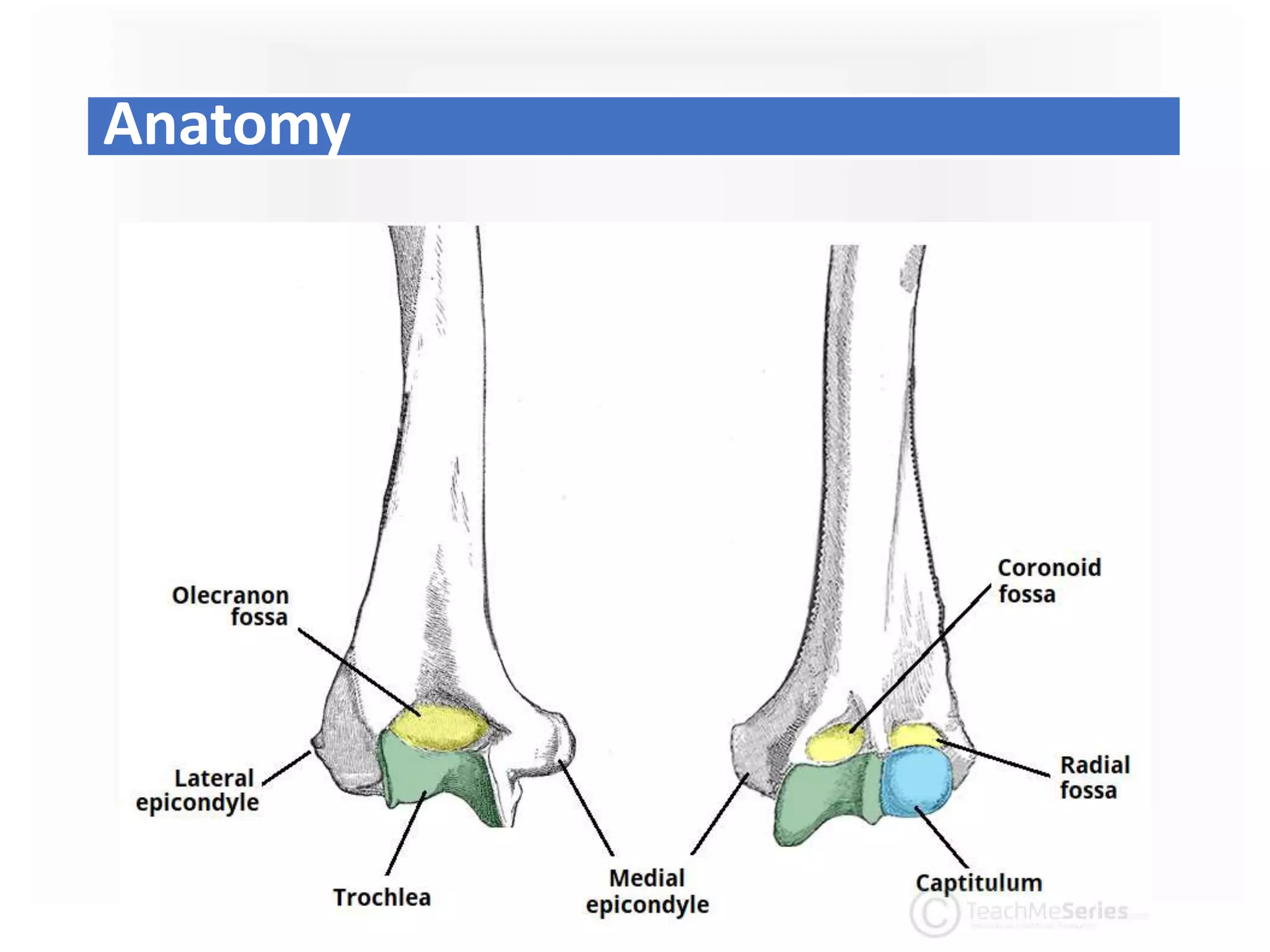
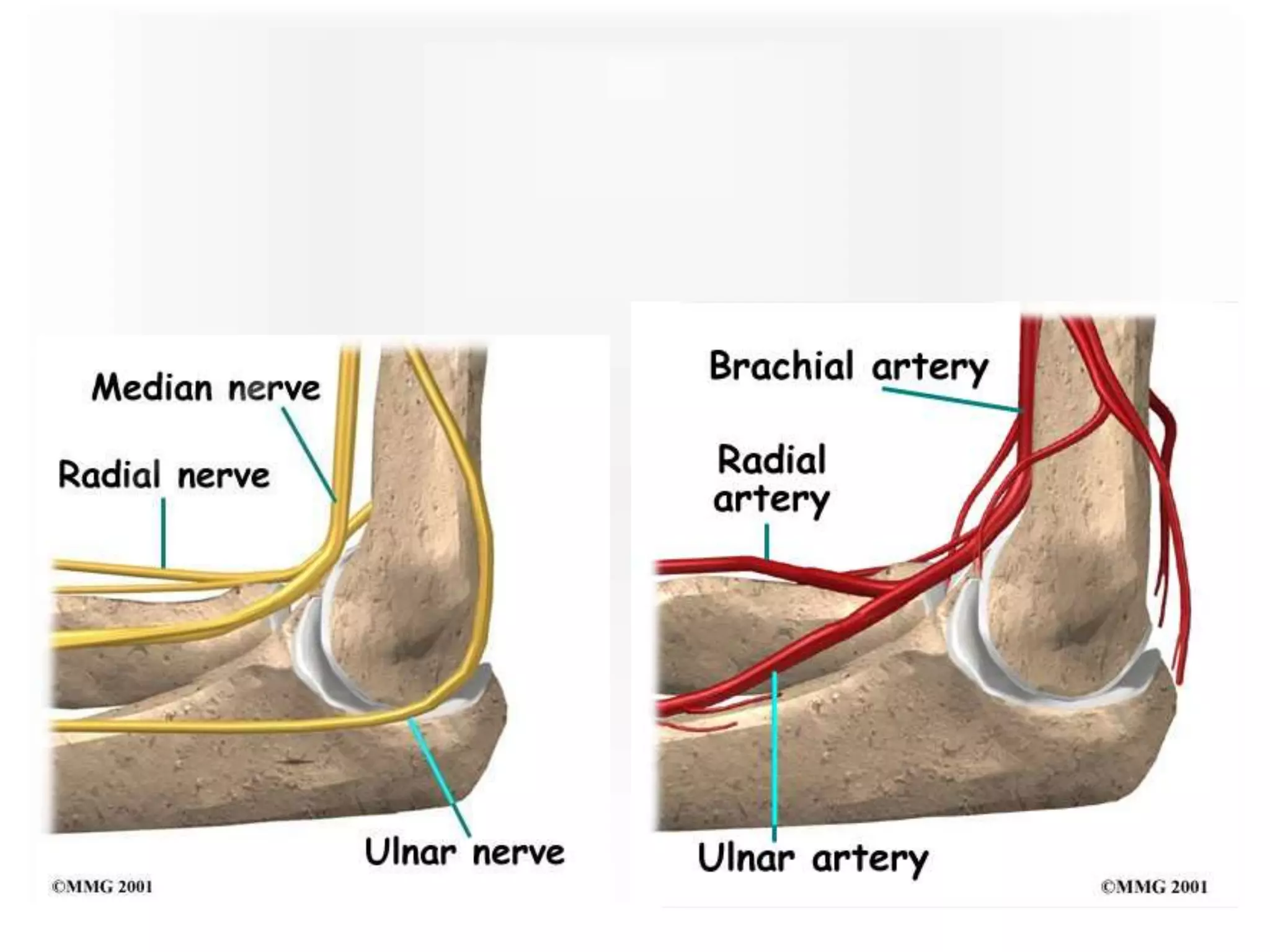
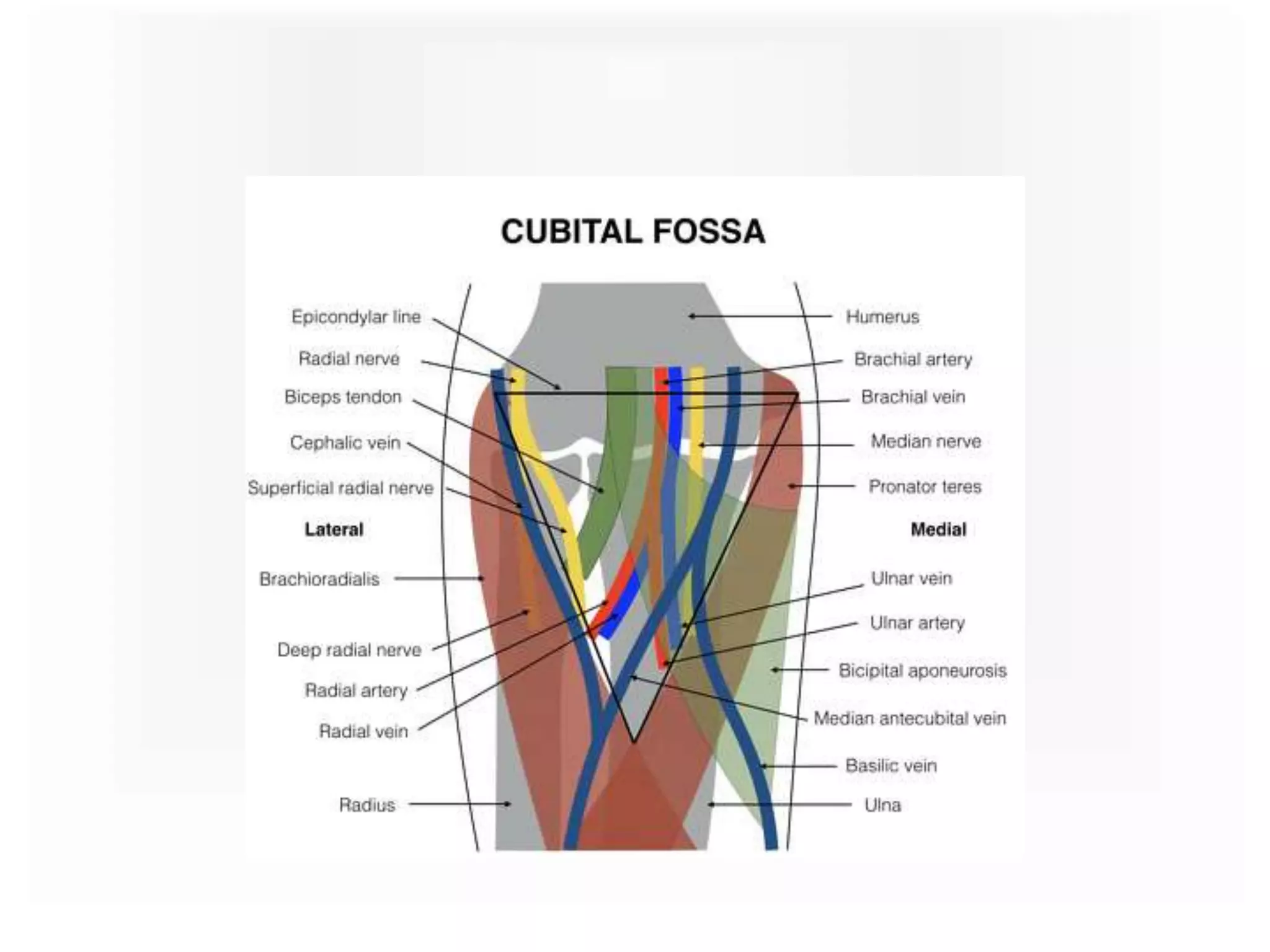
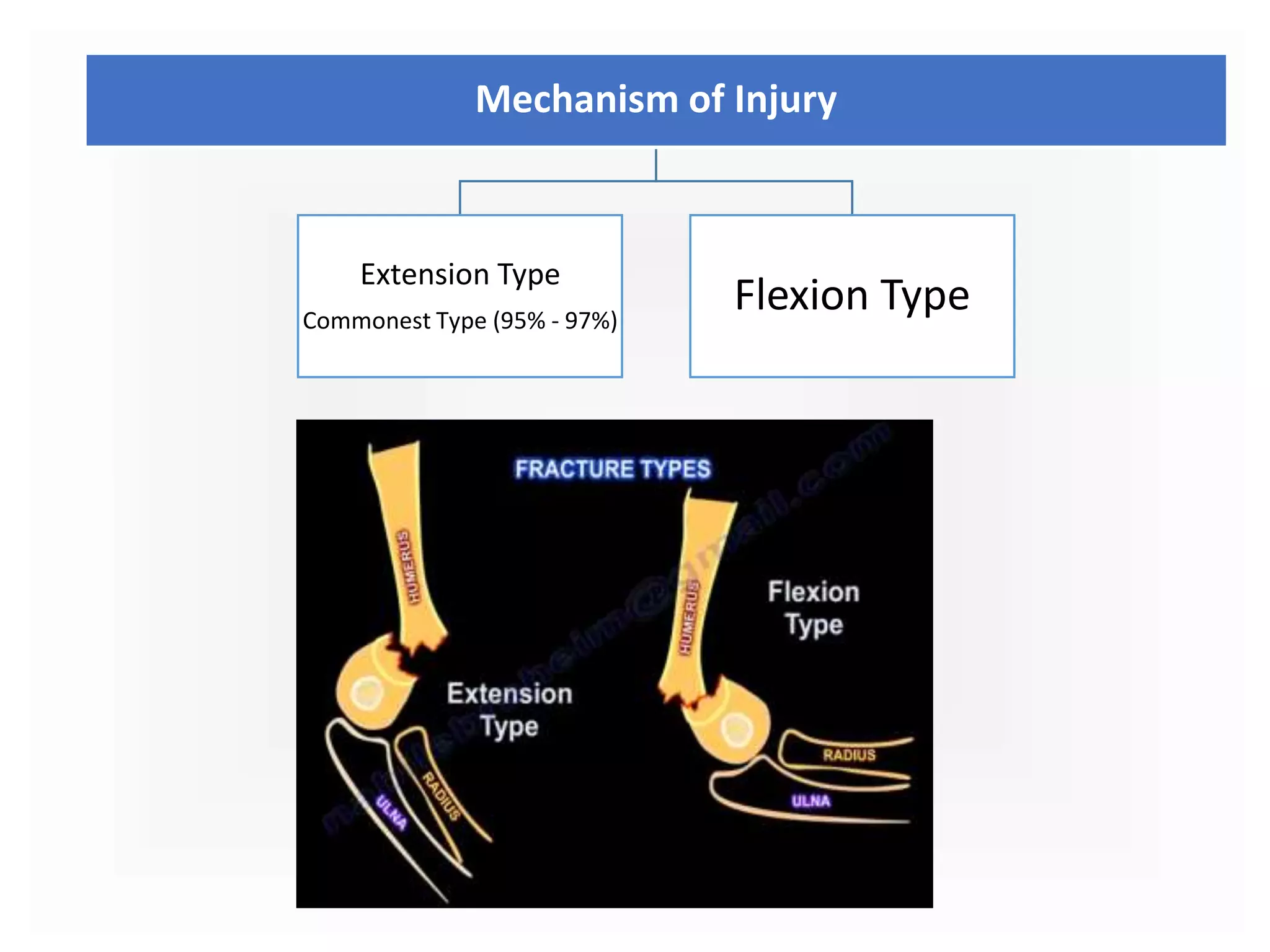
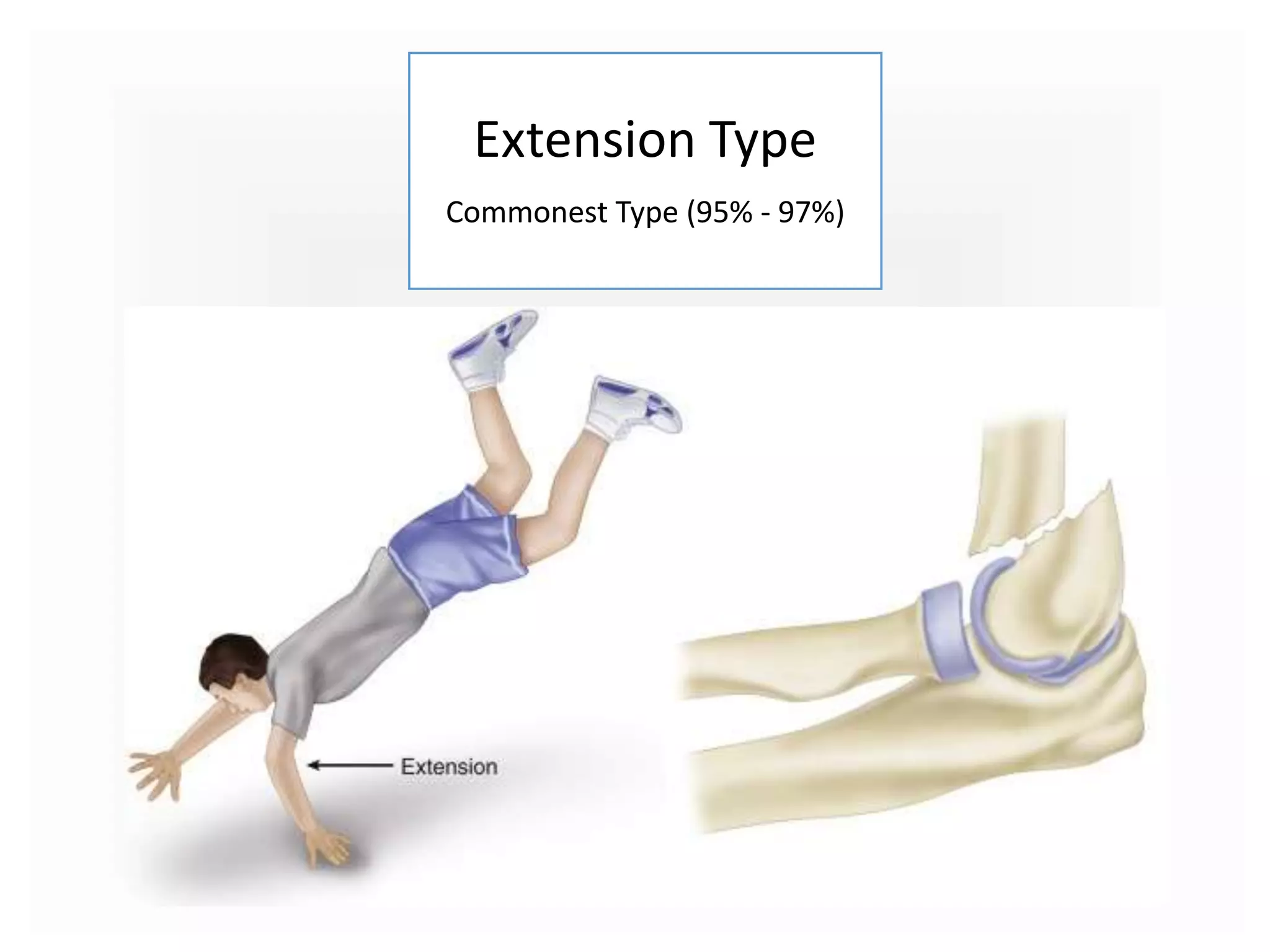
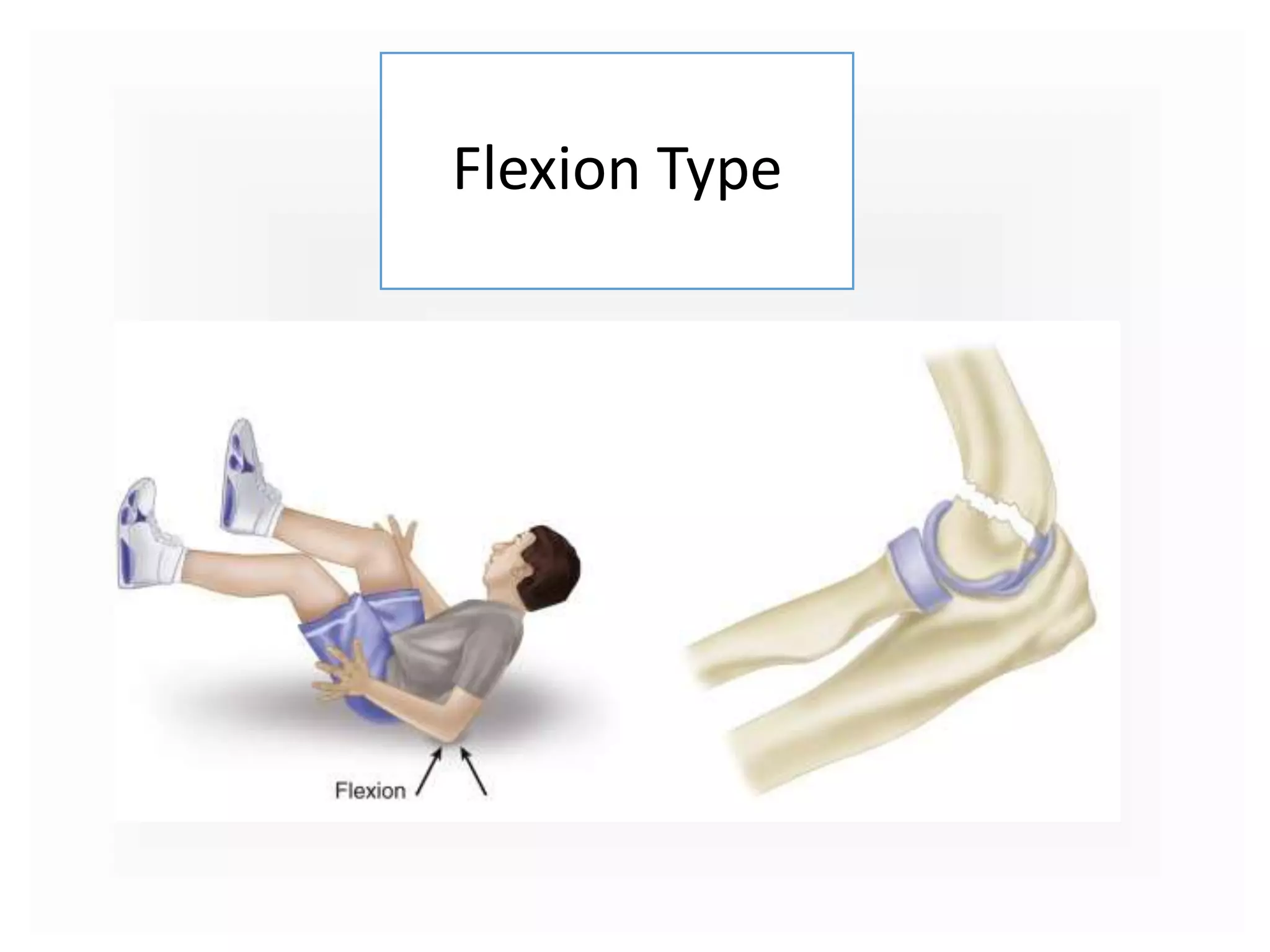
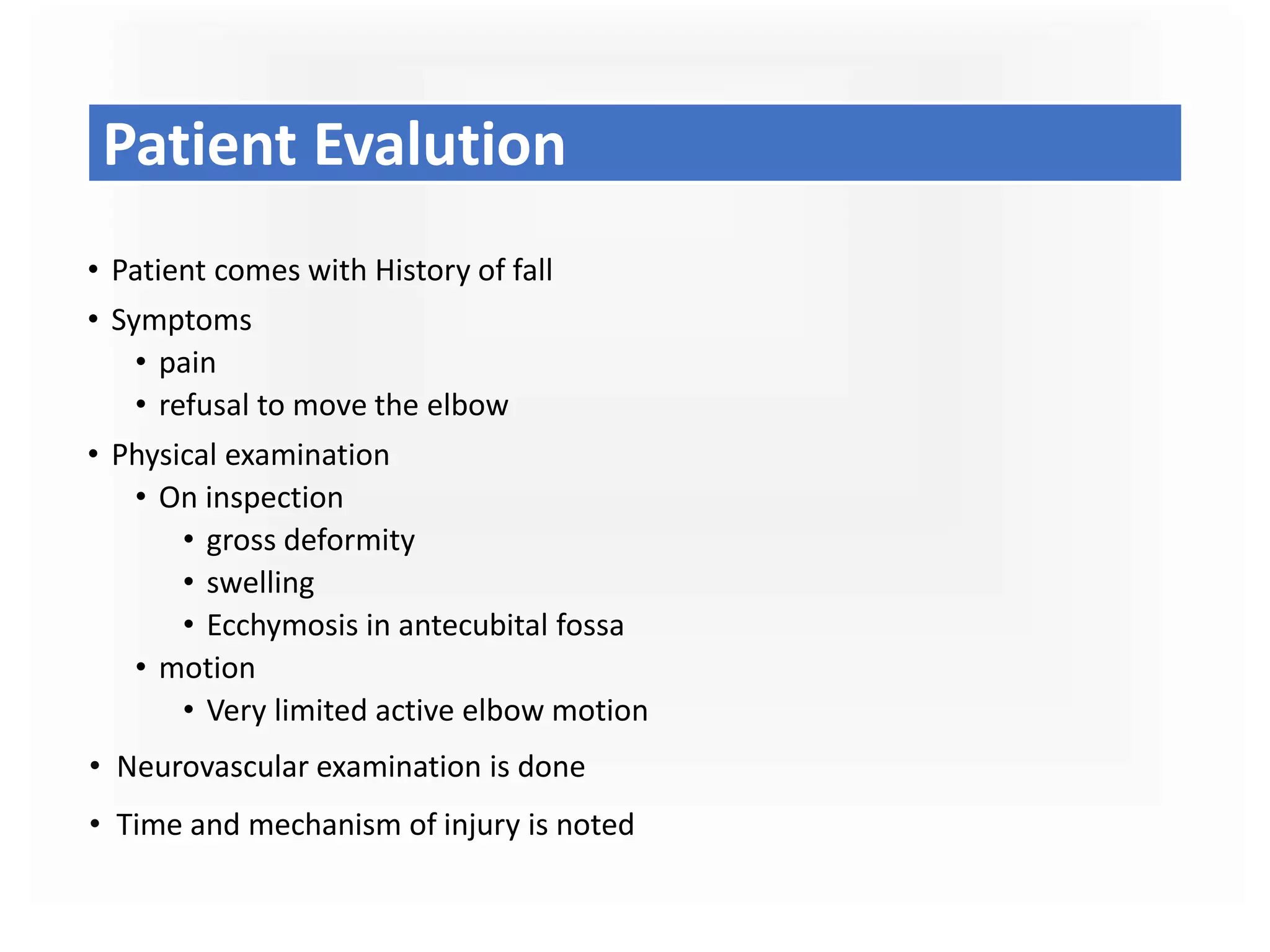
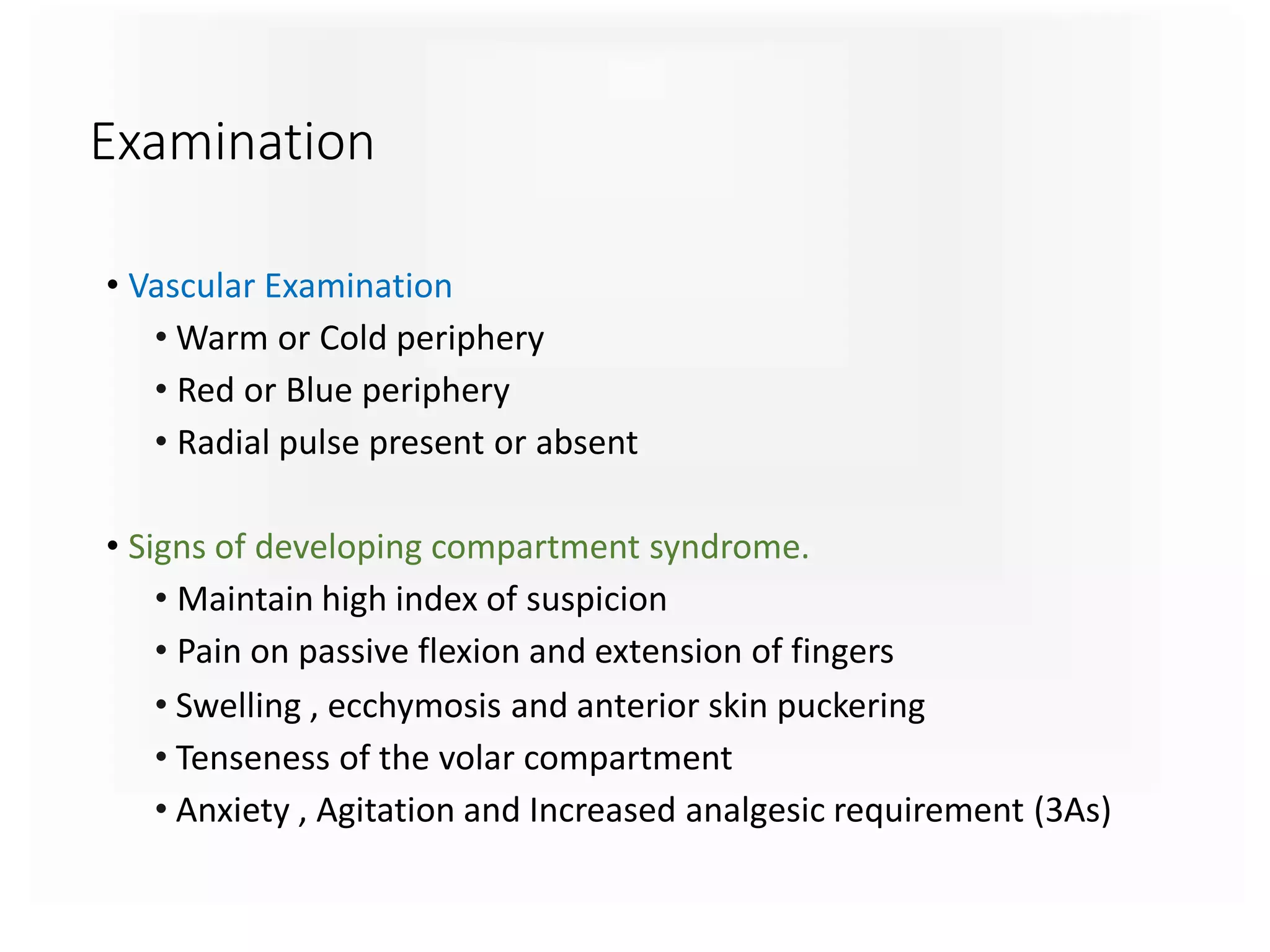
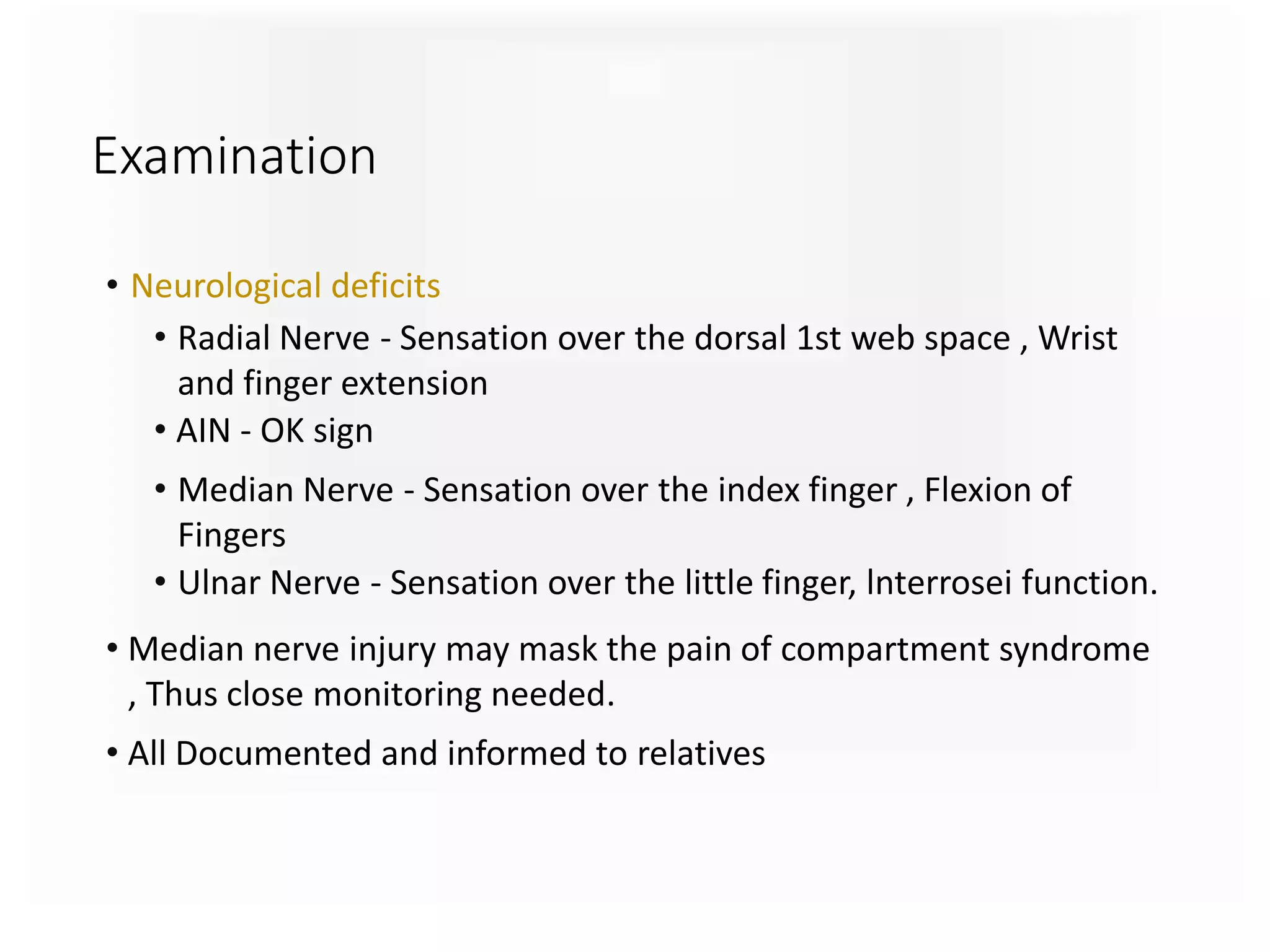
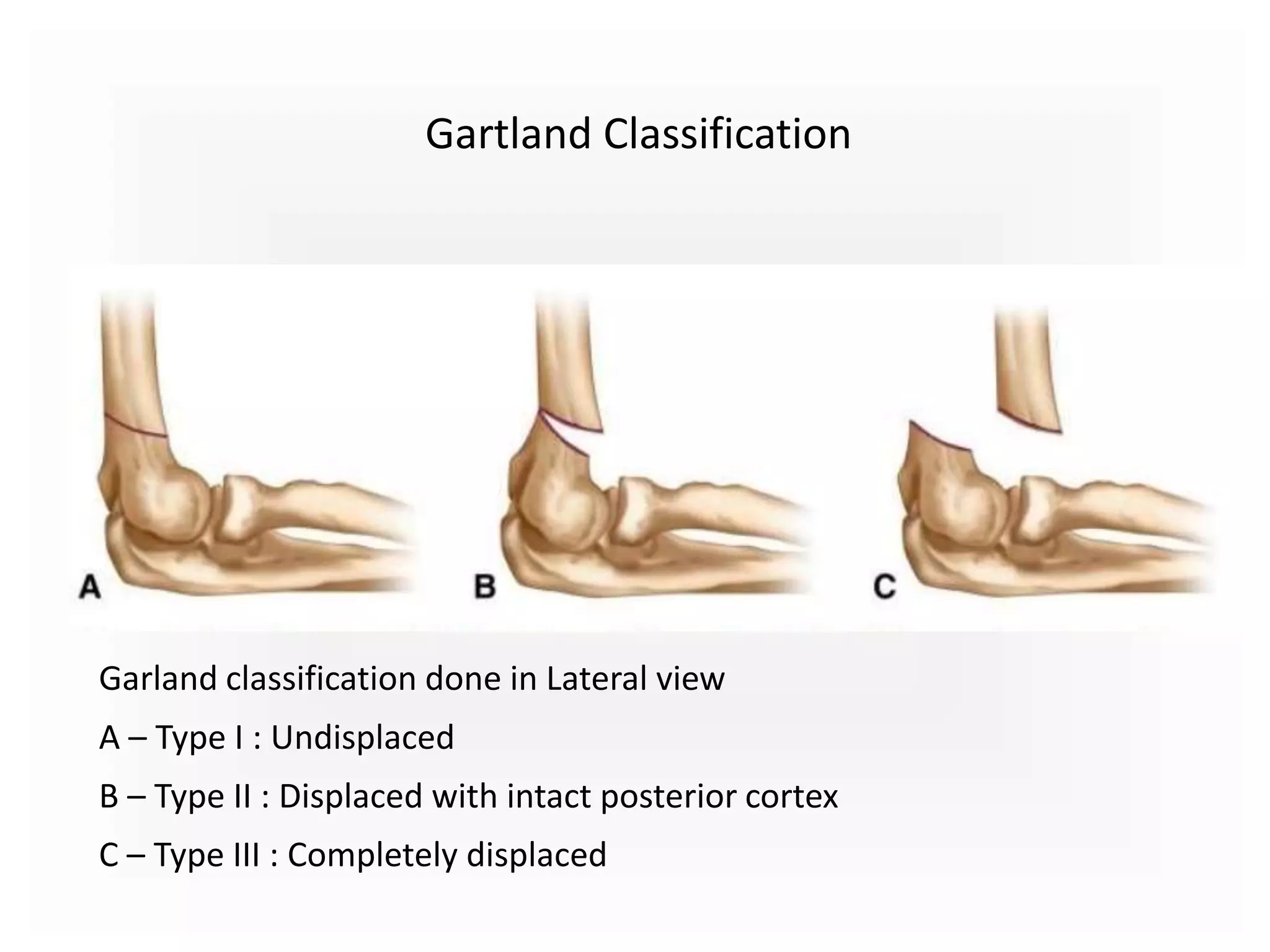
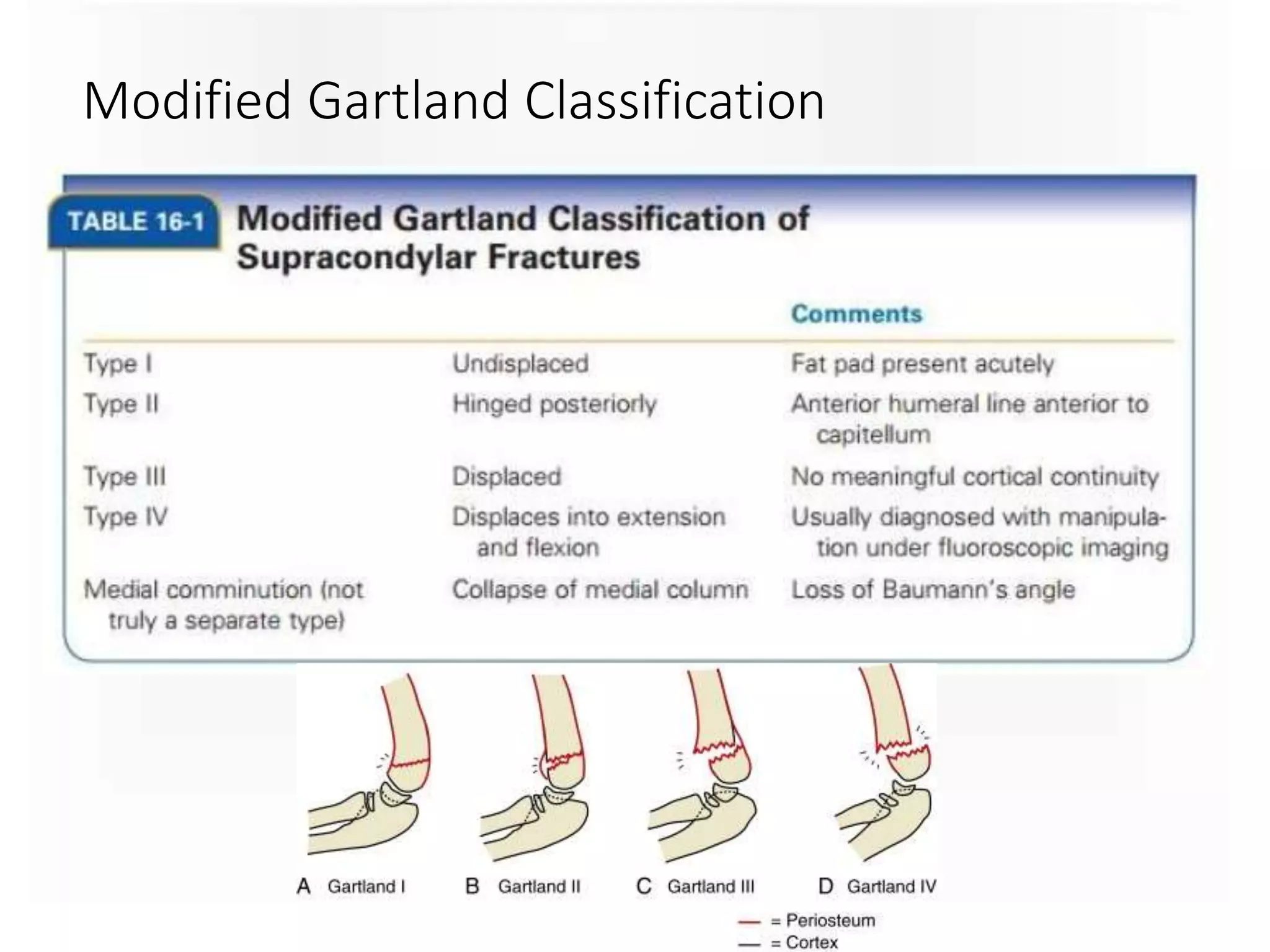
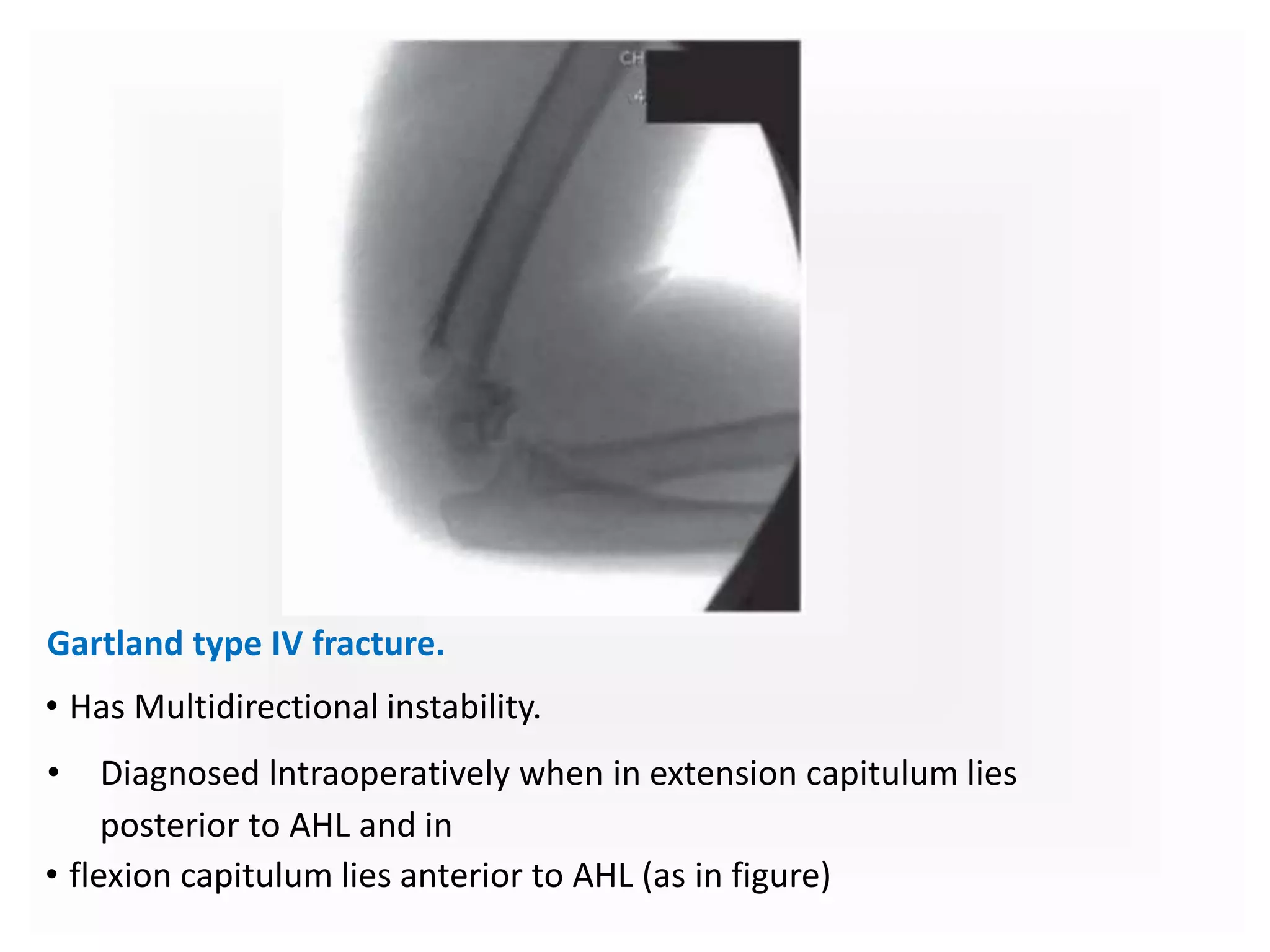
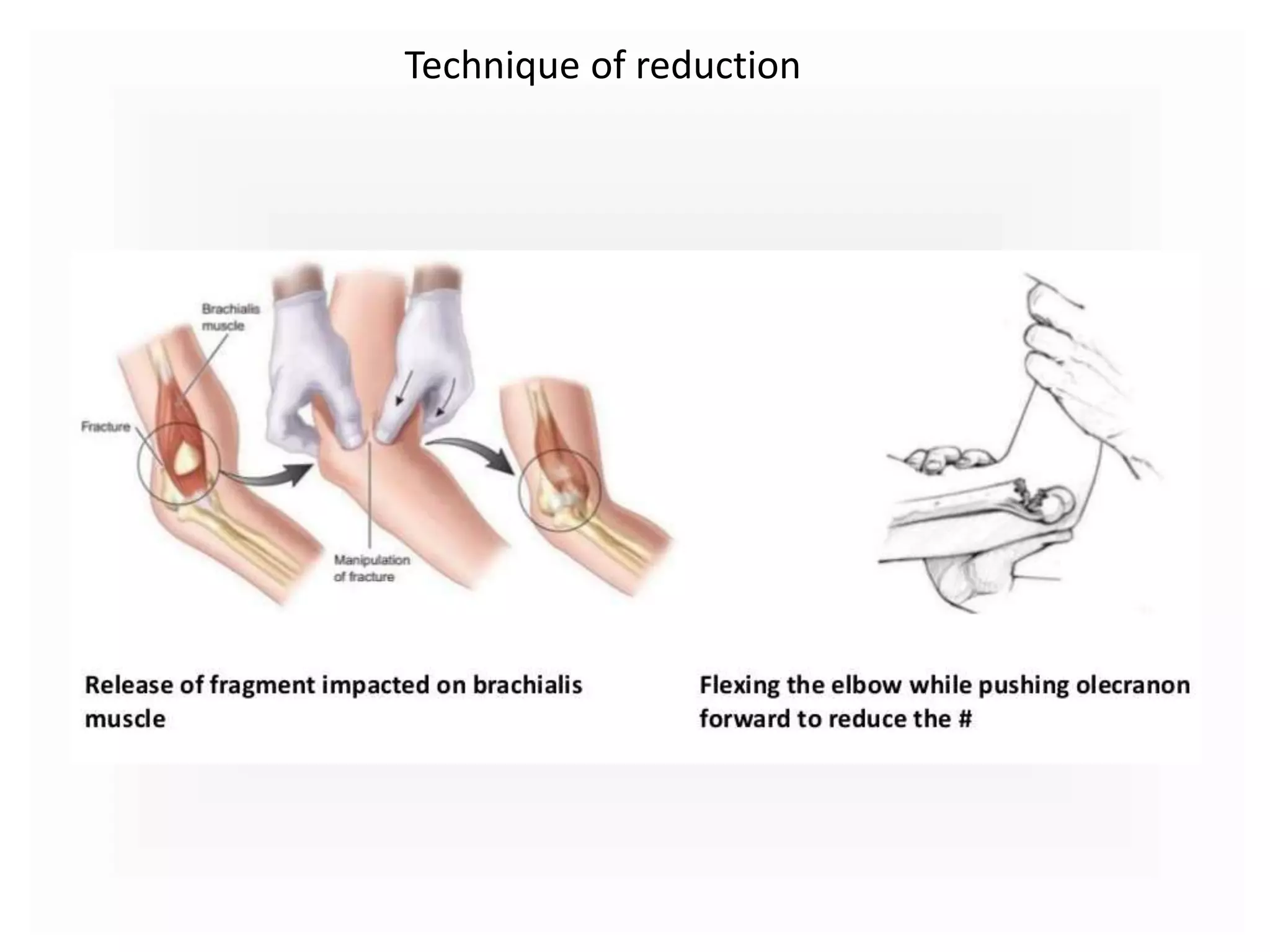
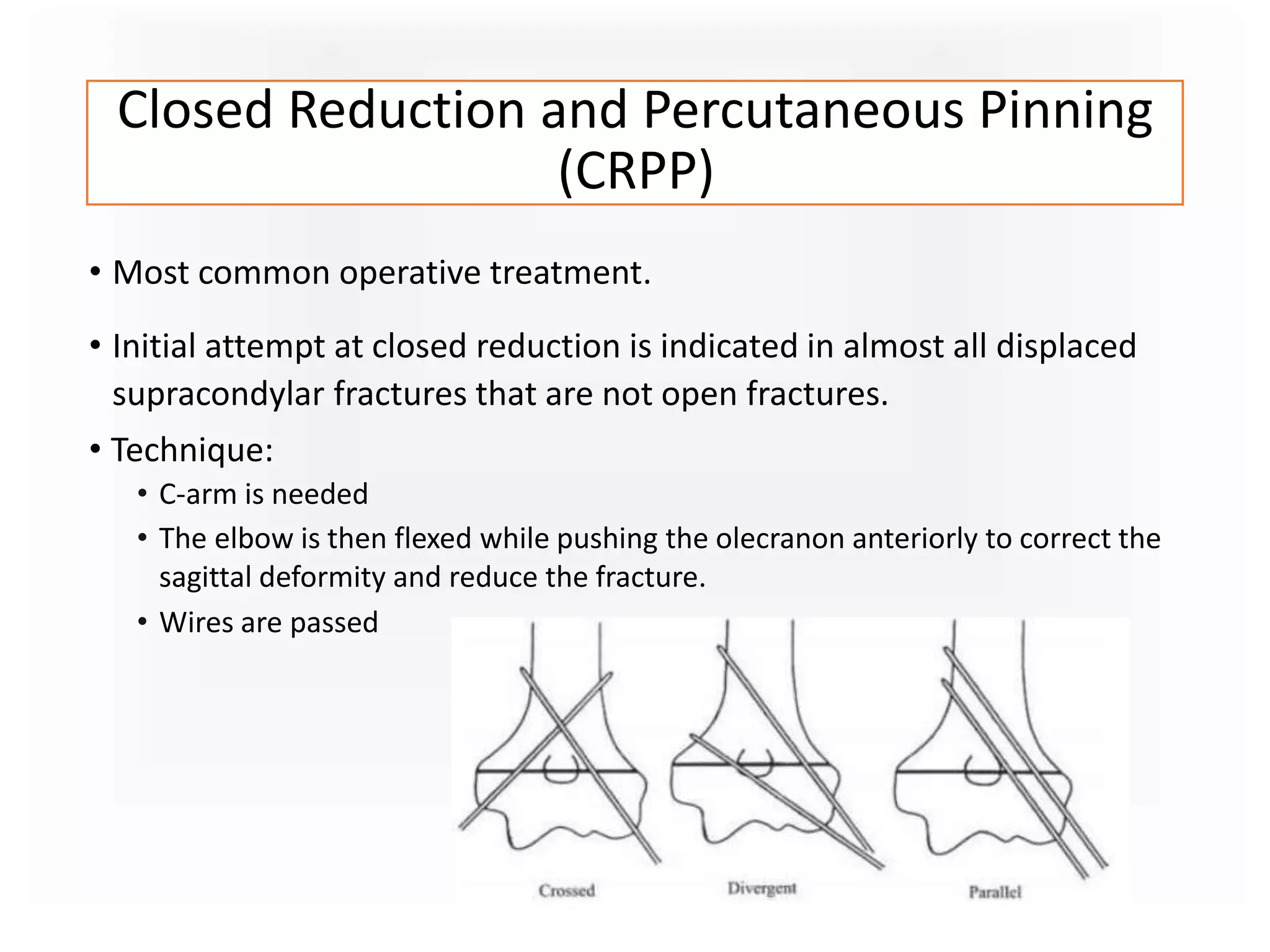
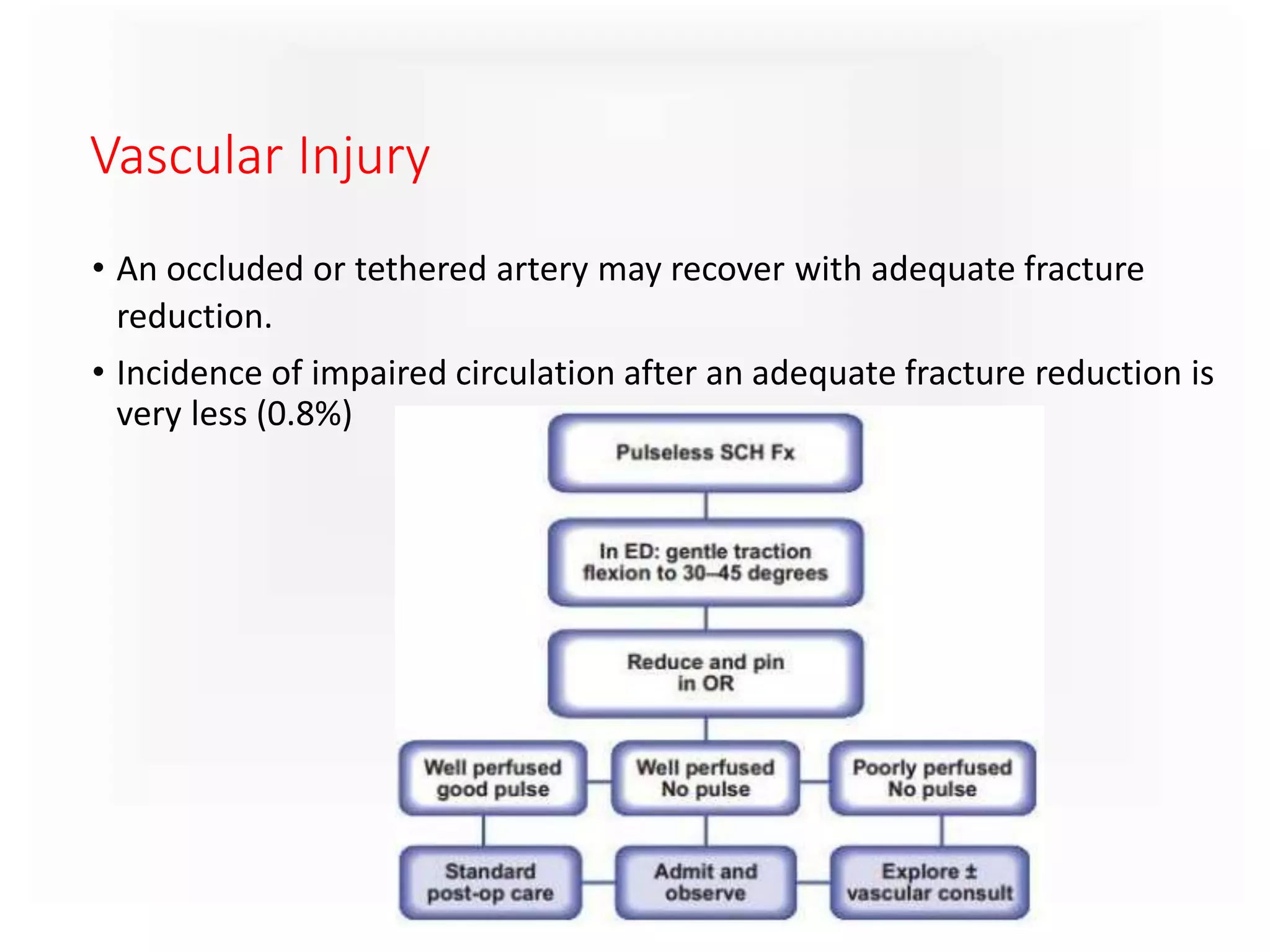
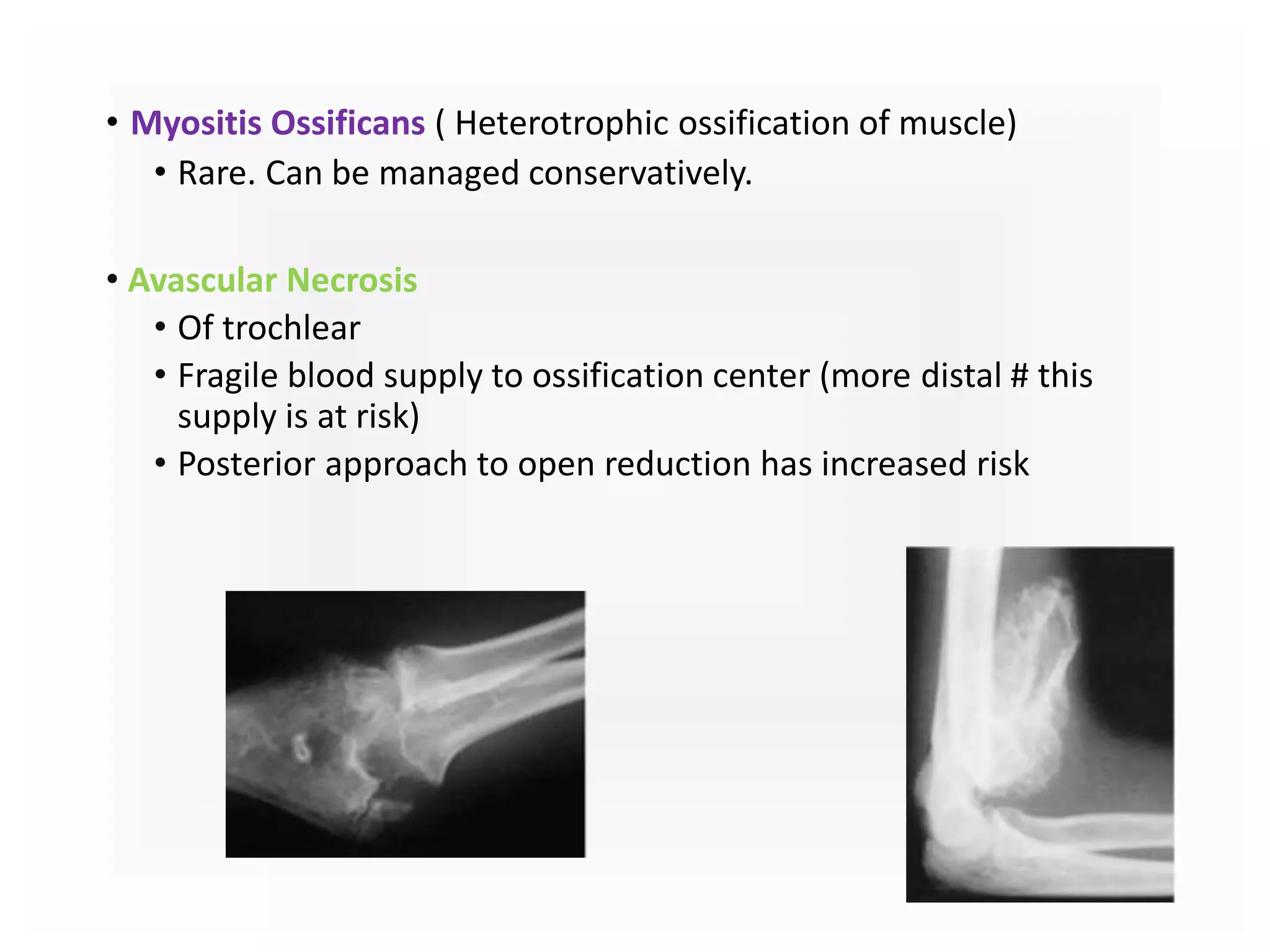
Supracondylar humerus fractures are the most common elbow injury in children, often occurring through a fall onto an outstretched hand. They are classified using Gartland or modified Gartland systems. Treatment depends on the degree of displacement but often involves closed reduction and percutaneous pinning. Complications can include nerve palsies, vascular injuries, compartment syndrome, malunion and stiffness. Close monitoring is important to prevent loss of reduction or complications.